Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/007
MINI REVIEW OPEN ACCESS
Anesthetic Considerations in Patients with Parkinson Disease and Deep Brain Stimulators
Kathryn Hall1 , MD
Kathryn Hall, M.D., Resident, Department of Anesthesiology and Critical Care, University of Pennsylvania. 3400 Spruce street, Philadelphia, PA, 19104, Email: Kathryn.Hall@uphs.upenn.edu
Received: May 01, 2014 | Accepted: June 01, 2014 | Published: July 01, 2014
Citation: Hall, Kathryn: Anesthetic Considerations in Patients with Parkinson's disease and Deep Brain Stimulators. Trans Periop & Pain Med 2014, 1(1):17~18.
Parkinson's disease is a neurodegenerative disorder of the central nervous system (CNS) clinically manifested by resting tremor, rigidity, bradykinesia, and postural instability. The pathology is characterized by loss of dopaminergic neurons within the pars compacta of the substantia nigra. Pharmacologic treatment centers on replacing this lost dopaminergic tone with levodopa, converted to dopamine in vivo. This is administered in conjunction with peripheral decarboxylase inhibitors (carbidopa) or catechol-o-methyltransferase (COMT) inhibitors (entacapone). Other therapies include other dopamine receptor agonists, type B monoamine oxidase (MAO) inhibitors and, in refractory cases, deep brain stimulation [1,2].
Common Perioperative Considerations
There are many perioperative considerations specific to patients with Parkinson's disease including, but not limited to, difficulties of airway management, autonomic dysregulation, and medication interactions. The muscles of the upper airway are also involved in the involuntary movement characteristic of the disease, which can subsequently cause poor handling of secretions and aspiration. These patients are predisposed to both laryngospasm and aspiration during induction of anesthesia and on extubation. Regional anesthesia is often preferred in this patient population given the airway challenges. The autonomic dysfunction seen in patients with Parkinson's disease, however, can be exacerbated by neuraxial anesthesia and close blood pressure monitoring is required. Levodopa has a short half life of 1-3 hours and is only available as an oral medication. In long cases it may be necessary to give this medication intraoperatively (via oro-gastric or nasogastric tube) to prevent onset of severe Parkinson symptoms after emergence [2]. If this is not feasible it is important to resume this medication as soon as possible post-operatively [2,3]. Patients with Parkinson's disease should not receive antidopaminergic medications such as phenothiazines (i.e. prochlorperazine), droperidol, or metoclopramide, as they may exacerbate extrapyramidal side effects.
Special considerations for Patients with Deep Brain Stimulators
Deep brain stimulators (DBSs) are increasingly being used to treat psychiatric and movement disorders. Patients with Parkinson's disease refractory to medical therapy can sometimes achieve some symptomatic benefit from these devices. DBS leads are carefully implanted in the brain (targeting the thalamus or basal ganglia) and connected to a pulse-generating device that is placed over the chest wall in a position similar to that used for cardiac pacemakers (on one side or both sides) [4,5]. Figure 1 demonstrates a stimulator on the left chest. There are several publications discussing the anesthetic management for DBS placement, however, there is a paucity of information on intraoperative DBS management for nonneurological procedures [5].
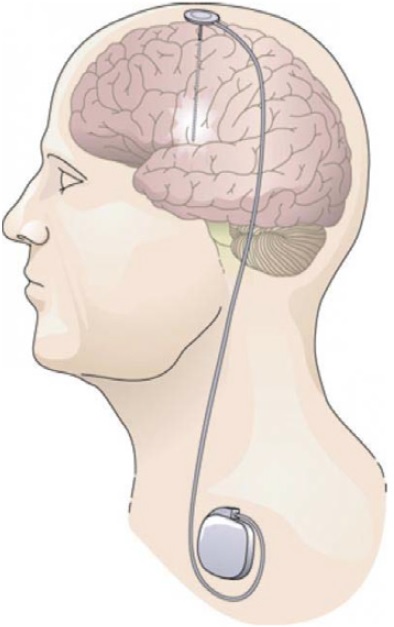
Figure 1: Battery powered deep brain stimulator is connected by extension wires to electrodes placed deep within the brain. Source: http://phys.org/news194718278.html#jCp
A pre-operative assessment of a DBS device should include understanding the original indication for placement, how long it has been in place, and what effect the device has had on severity of symptoms. According to the Medtronic DBS Sales Department, it is recommended that all patients who have the Medtronic Ativa platform devices bring their patient programmers (resembles a remote) with them to the hospital on the day of the procedure, as these devices are unlike pacemakers and automated implantable cardioverter-defibrillators (AICDs) and not designed to respond to placement of an external magnet. Similar to AICDs and pace-makers, however, there is a theoretical risk that electrocautery could damage the DBS leads or pulse generating device. This could potentially result damage to the device's internal circuitry or programming, damage to the leads, or even permanent CNS injury. As a precaution, bipolar electrocautery should be used when possible and grounding pads should be placed close to the surgical site. The device may also interfere with ECG tracing and limit ECG interpretation [6,7].
The manufacturer's recommendation is that the DBS device be switched off during surgery. However, one must be cognizant of minimizing the length of time that the device is turned off so as to limit the severity of Parkinson symptoms after emergence.According to Medtronic DBS Consultant (personal email communication), if the patient has severe underlying symptoms it may be best to turn off the device after induction of general anesthesia. If turned off prior to induction the patient may develop dyskinesias, which may make interventions such as endotracheal intubation and vascular access more difficult. Careful attention should be paid to patient positioning, as neck manipulation can interfere with and possibly damage the DBS device leads. The device should be turned on again prior to emergence to not only facilitate a smooth extubation but also to minimize patient suffering of Parkinson symptoms after emergence [6].
References
- Tinklepaugh MS. Chapter 29 Parkinson's disease. In Atchabahian A, Gupta R (2014) The Anesthesia Guide. 109-111.
- Nicholson G, Pereira AC, Hall GM (2002) Parkinson's disease and anaesthesia. Br. J. Anaesth. 89: 904-916.
- Gálvez-Jiménez N, Lang AE (2004). The perioperative management of Parkinson's revisited. Neurol Clin. 22: 367-377.
- Deiner S, Hagen J (2009) Parkinson's disease and deep brain stimulator placement. Anesthesiology Clinics. 27: 391-415.
- Venkatraghavan L, Luciano M, Mannien P (2010) Anesthetic management of patients undergoing deep brain stimulator insertion." Anesthesia Analgesia. 110: 1138-1145.
- Garg, R, Borthakur B, and Pawar M (2011) Management of patient with deep brain stimulator for emergency laparotomy. J Neurosurg Anesthesiol 23:168.