Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/049
RESEARCH ARTICLE OPEN ACCESS
Spinal Cord Stimulation versus Other Therapies in Patients with Refractory Angina: A Meta-analysis
Shaocheng Wang a,b ,Qixian Li c, Hongwei Fangd , Hao Yang b, Diansan Su d, Yuan-Xiang Taoe, Zhankui Wang b, Xiangrui Wang b , Zhongwei Yang d
aDepartment of Anesthesiology, Bengbu Medical College
bDepartment of Pain Management, South Compus, Renji Hospital, School of Medicine, Shanghai Jiaotong University
cDepartment of Pediatrics, Shili Hospi- tal
dDepartment of Anesthesiology, Renji Hospital, School of Medicine, Shanghai Jiaotong University
eDepartment of Anesthesiology, New Jersey Medical School, Rutgers, The State University of New Jersey
Authorship note: Shaocheng Wang and Qixian Li contribute equally to this work.
XiangRui Wang, Ph.D, M.D, Department of Pain Management, South Compus, Renji Hospital, School of Medicine, Shanghai Jiaotong University, 2000 Jiangyue Road, Shanghai 201114, China. Tel.: + 86 21 58752345; fax: +86 21 58752346, E-mail: xiangruiwang2016@163.com; ZhongWei Yang, Ph.D, Department of Anesthesiology , Renji Hospital, School of Medicine, Shanghai Jiaotong University, 1630 Dongfang Road, Shanghai 200127, China. Tel.: + 86 21 68383198; fax: +86 21 50903239, E-mail: yangzhongweitcm@163. com
Editor: Henry Liu, MD. Clinical Professor of Anesthesiology, Department of Anesthesiology, Hahnemann University Hospital, Drexel University College of Medicine. 245 N. 15th Street, MS 310, Philadelphia, PA 19102, USA, Phone: (215)762-7877, Email: henryliupa@gmail.com
Received: November 16, 2016 | Accepted: January 20, 2017 | Published: January 31, 2017
Citation: Wang S, Li Q, Fang H, Yang H, Su D, Tao YX, Wang Z, Wang X, Yang Z. Spinal cord stimulation versus other therapies in patients with refractory angina: A meta-analysis Transl Perioper & Pain Med 2017; 2(1): 31-41.
Background
An increasing number of patients with coronary disease suffer from angina that cannot be controlled by optimal medical management and revascularization. The purpose of this study was to evaluate the method of spinal cord stimulation (SCS) for the treatment of patients with refractory angina (RA).
Methods
We searched multiple databases, including PubMed, EMBASE, the Cochrane Library, and the Cochrane Central Register of Controlled Trials. The results of studies through March 2016 were included in our analyses. Systematic methodological appraisal and data extraction were conducted by two independent reviewers. All data analyses utilized the Review Manager 5.3, and the results were merged as weighted mean differences (WMD).
Results
Nine randomized controlled trials (RCTs) with a total of 364 patients who were diagnosed with RA were included in the analysis. After being pooled, the outcomes from the SCS treatment group did not differ from those from the coronary artery bypass grafting (CABG) or percutaneous myocardial laser revascularization (PMR) treatment groups. However, compared with ‘no SCS stimulation' treatment groups, SCS significantly decreased nitrate drug usage (WMD: -2.03, 95% CI: [-3.12, -0.93], p=0. 0003) and increased several indicators of healthrelated quality of life (HRQOL).
Conclusions
SCS appears to be a safe and effective management for RA although, it has similar efficacy when compared to PMR or CABG as a potential replacement therapy. However, before this method is used as a conventional treatment, more high-quality designed multicenter RCTs are needed.
Keywords
Refractory angina; Coronary disease; spinal cord stimulation, Clinical Trail, Meta-analysis
Introduction
Refractory angina is a type of coronary artery disease caused by coronary insufficiency that cannot be controlled by drug therapy, angioplasty and CABG; patients with RA face serious clinical problems. The clinical symptoms o RA are caused by reversible myocardial ischemia [1]. It has been estimated that approximately 350,000 patients each year are diagnosed with RA [2]. These patients mainly have severe physical limitations and a higher risk of heart attack, which reduces their quality of life despite optimal drug treatment. Various treatments for RA have been studied, such as spinal cord stimulation (SCS) [1, 3], enhanced external counterpulsation (EECP), CABG and PMR.
The SCS has been developed based on the "Gate control theory" [4] in which the segmental pain is inhibited. After the SCS was first implanted in the patients in 1967 [5], SCS was first used for RA in 1987 [6].
SCS was implanted at the level of the 6-8th thoracic vertebrae via an incision under anesthesia. Next, an electrode was inserted into the epidural space and advanced up to the 1st -2nd thoracic vertebrae under fluoroscopic guidance. Its location was adjusted up to the level where the patient experienced paresthesia and commensurate with the angina pain site. An extended wire was attached to a subcutaneous pulse-generator through an incision in the left side of the flank that was below the left costal arch. A typical therapy for SCS is a low-amplitude stimulation three times per day for 1 hour in addition to using a strong stimulation during an angina attack. Patients can control the intensity of the stimulation when they feel pain. This method was recommended by the European Society of Cardiology (ESC) [7], the American Heart Association (AHA) and six additional scientific associations [8]. Here, we proceeded with a meta-analysis to evaluate the efficacy and safety of SCS for patients with RA.
Methods
Electronic literature search strategy
We searched several electronic databases including EMBASE, The Cochrane Library, MEDLINE, and The Cochrane Central Register of Controlled Trials from their inception to March 2016 for the selection of related articles. Our search terms included "spinal cord stimulation" and its synonyms, "refractory angina" and its synonyms, and the two terms combined. The electronic databases were searched by two independent investigators (Shaocheng Wang and Qixian Li). The abstracts of all articles identified as potentially related were retrieved and examined in the study selection process. Repetition of published trials was included only once.
Inclusion criteria
Studies qualified for inclusion if they were RCTs that included patients who were diagnosed with RA using predefined clinical criteria as well as those who received SCS therapy (whether alone or combined with other treatments). Reviews, observation studies, case reports, articles not relating to either SCS or refractory angina, and articles about SCS in syndrome X were excluded.
Data extraction and risk of bias assessment
Data extraction and risk of bias assessment were carried out by two independent investigators, with any disagreements being settled by a third investigator (Xiangrui Wang). We extracted the following outcome categories: exercise capacity, ischemic burden, anti-angina drug consumption, safety (morbidity, and SCS relevant complications), Canadian Cardiovascular Scale (CCS) class change and HRQOL.
We used Review Manager software (RevMan, version 5.3) to construct 'the risk of bias' (Figure 1) and included six parameters of bias with each parameter divided into "high risk ", "low risk", or "unclear risk". This was evaluated by the same two independent reviewers.
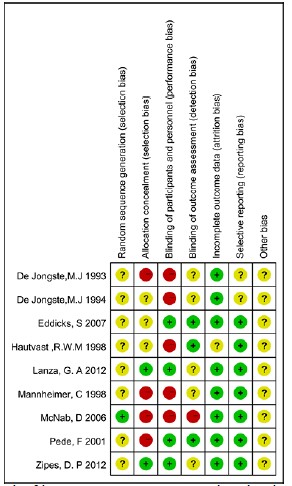
Figure 1: Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Data presentation and analysis
Nine RCTs, which included 364 patients with RA, were used in this meta-analysis. These studies were separated into two categories: SCS vs active intervention (CABG or PMR) [9, 10] and active SCS (SCS ON) vs no or inactive SCS (SCS OFF) [11-17]. Quantitative data was then entered into the Cochrane RevMan5.3 software. All results were converted into mean ± standard deviation (SD). We translated data reported only as median, size, and range into mean ± SD using a method previously reported[18]. Results were recorded as WMD with a 95% confidence interval (CI). In addition, the WMD was considered statistically significant if the 95% CI was not equal to 0.
Results
Study characteristics
We searched the electronic databases using the keywords and their synonyms. After checking the titles and abstracts, 109 relevant studies were initially selected. Thirty-nine repeated studies and 27 non-RCT records (including 24 reviews, 2 meta-analyses, and 1 case report) were excluded. In addition, 34 full-text articles were excluded because they were not related to RA or SCS or had inappropriate intervention (Figure 2). Ultimately, nine studies, which included 364 patients, were analyzed in the present study.

Figure 2: Summary of study selection and exclude process.
Patients were divided into three SCS groups according to the previous report [15]: control (24 h/day with 0 output), 3 × 2 h/day or 24 h/day with conventional output and 3 × 2 h/day with a subthreshold output. We chose the results of 3 × 2 hours/day as the SCS group in the present study. The characteristics of the identified studies are presented in Table 1.
Table 1: Characteristics of RCTs included in the meta-analysis
| Included of studies Country /year Design |
Age-Mean (SD or range) Sex-% male Class Inclusion criteria |
Intervention | Outcomes | Follow up | |
|---|---|---|---|---|---|
| N patients | N patients | ||||
| De Jong, M.J Netherlands/1993 single-center RCT |
60.3 years (5) 70.8%male NYHA class III/IV Not suitable for revascularization 18-76 years |
SCS ON N=12 |
SCS OFF N=10 |
Quality of life. Exercise capacity (treadmill time) Nitrate consumption |
1 year |
| De Jong, M.J Netherlands/1994 Single-center RCT |
62.8 years (3.1) 88.2%male NYHA class III/IV Not suitable for revascutarizatian procedures Reversible ischemia on exercise Receiving optimal drug therapy |
SCS ON N=8 |
SCS OFF N=9 |
Exercise (treadmill time) Health-related quality of life Nitrate drug usage Ischemic burden |
6-8weeks |
| Hautvast, R.W.M Netherlands/1998 Single-center RCT |
62.5 years (7.5) 56%male NYHA class III/IV Not suitable for revascularization procedures Receiving optimal drug therapy |
SCS ON 13 |
SCS OFF 12 |
Angina attacks Nitrate consumption Exercise (treadmill time) Health-related quality of life |
6 weeks |
| Mannheimer, C Sweden/1998 Single-center RCT |
68.9 years (40-82) 80%male AHA angina class 3/4 Symptomatic indication for CABG and no benefit from CABG |
SCS N=53 |
CABG N=51 |
Exercise capacity (workload time), Nitrate consumption Angina attack frequency Adverse events |
6 months 2 years 5 years |
| Pede, F Italy/2001 Single-center Cross Over RCT |
76 years (8) 60%male CCS class 3/4 Not suitable for revascularization procedures Reversible ischemia on exercise |
SCS ON 15 |
SCS OFF 15 |
Ischemic burden | 48h |
| Eddicks, S., Germany/2007 Single-center Cross Over RCT |
65 years (8) 67%male CCS class 3/4 Angina pectoris >3 months Known coronary artery disease Reversible myocardial ischemia Optimal antianginal medication No benefit from revascularization |
SCS1 N=12 |
SCS 2 N=12 |
Six-minute walk test Quality of life Angina attacks Nitrate usage CCS angina classification |
4 weeks |
| McNab, D UK/2006 Single-center RCT |
63.6 years 88%male CCS class 3/4 |
SCS N=34 |
PMR N=34 |
Exercise (treadmill time) Change in CCS Quality of life Adverse events |
3 months 12 months 24 months |
| Lanza, G. A Italy/2012 Multicenter RCT |
68 years (11.8) 52%male CCS class 3/4 Reversible myocardial ischemia Unsuitable for surgical and percutaneous coronary artery revascularization Stable picture of angina in the 2 months |
SCS ON 10 |
SCS OFF 8 |
Angina episodes Nitrate consumption CCS angina class VAS score |
1 month 3 months |
| Zipes, D. P USA/2012 Multicenter RCT |
61.1 years (10.7) 73.5%male CCS class 3/4 Stable angina for two months Not a candidate for CABG or PCI Refractory angina despite optimal/maximal medical treatment |
SCS ON 32 |
SCS OFF 36 |
Exercise capacity (treadmill time) Angina attacks Nitrate usage CCS class change Angina frequency Adverse Events |
6 months |
*: 1 stimulation for 3 × 2 h/day with conventional output
2 stimulation for 24 h/day with 0.1 V output
*: CCS: Canadian Cardiovascular Scale; AHA: American Heart Association; NYHA: New York Heart Association:
CABG: coronary artery bypass graft; PMR: percutaneous myocardial laser revascularization.
Nitrate drug usage
Six studies [10, 11, 13-15, 17] presented data on nitrate drug usage. As shown in
Figure 3, five studies compared 'SCS ON' with 'SCS OFF', which had a significant reduction in nitrate drug usage following SCS (WMD: -2.03, 95% CI: [3.12, -0.93], p=0.0003). However, the χ2 and I2 were 16.27 and 75%, respectively, which suggested heterogeneity among the studies. One study compared SCS with CABG, and this difference was not statistically significant.
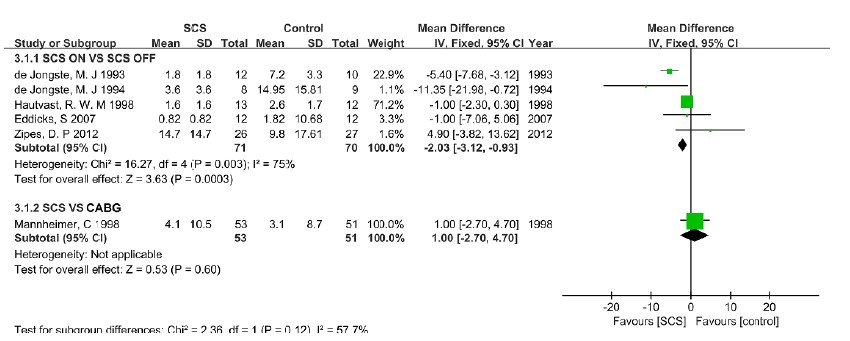
Figure 3: Forest plot of nitrate drug usage – differences among groups.
Exercise capacity
Six [9-11, 13, 14, 17] of the included studies provided data on exercise capacity (treadmill time and peak workload). Of the four studies comparing 'SCS ON' with 'SCS OFF', the pooled analysis showed a higher level of exercise capacity following SCS (WMD: 0.38, 95% CI: [-1.57, 2.34], p=0.7, Test of heterogeneity: χ2=6.44, I2=53%, p=0.09), but the difference was not statistically significant. No difference was found between SCS and CABG or PMR (Figure 4).
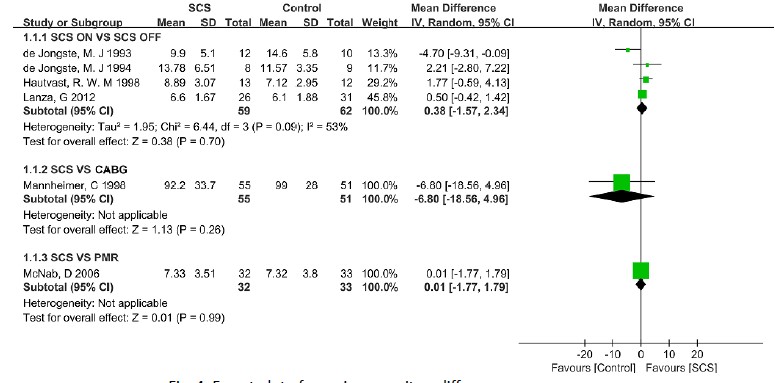
Figure 4: Forest plot of exercise capacity – differences among groups.
Ischemic burden
Four outcomes (angina attack frequency, magnitude of ST-depression, Time to angina, and visual analogue scale) were included in the ischemic burden group. Angina attack frequency was reported in seven studies. Of the six studies that compared 'SCS ON' with 'SCS OFF' [11, 13, 14, 16, 17], the pooled analysis exhibited a lower level of angina attack frequency following SCS (WMD: -2.85, 95% CI: [-5.78, 0.09], p=0.06, Test of heterogeneity: χ2 =2.65, I2 =0%, p=0.75), and no difference was found between SCS and CABG for angina attack frequency [10](Figure 5A).

Figure 5: Forest plot of ischemic burden – differences among groups: (A) angina attack frequency, (B) ST-depression, (C) time to angina, (D) Visual analogue scale.
Four studies presented data on the magnitude of STdepression; three of these studies compared 'SCS ON' with 'SCS OFF' [11, 12, 14] and there were no significant differences in the two groups (WMD: -0.01, 95% CI:[0.06, 0.05], p=0.8, test of heterogeneity: χ2 =0.36, I2 =0%, p=0.8). When comparing SCS to CABG, there was a significant increase in ST-depression [10](WMD: 0.13, 95% CI: [0.08, 0.18], p< 0.00001) (Figure 5B).
Five studies provided data on Time to angina. Four of these studies compared 'SCS ON' with 'SCS OFF' [11-14], and in addition, one study compared SCS with PMR [9]. No statistical significance was found for Time to angina when comparing 'SCS ON' with 'SCS OFF' (WMD: 0.21, 95% CI: [-1.5, 1.92], p=0.81, test of heterogeneity: χ2=8.54, I2 =65%, p=0.04). There was also no difference in Time to angina when SCS was compared to PMR (Figure 5C).
VAS was recorded in three studies [14, 15, 17], and the pooled analysis did not demonstrate statistical significance when comparing 'SCS ON' to 'SCS OFF' (WMD: -0.04, 95% CI: [-0.73, 0.66], p=0.91, test of heterogeneity: χ2 =2.47, I2 =19%, p=0.29) (Figure 5D).
Health-related quality of life
Five studies presented data on HRQOL including the daily activity score (ADL), social activity score (SAS), and Seattle Angina Questionnaire (SAQ). ADL was recorded in two studies [11, 13] that compared 'SCS ON' with SCS OFF', but the pooled analysis did not achieve statistical significance (Figure 6A).
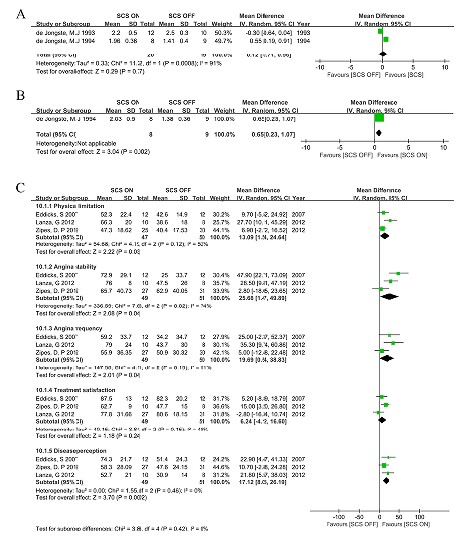
Figure 6: Forest plot of health related quality of life – difference among groups: (A) Daily activity score, (B) Social activity score, (C) Seattle Angina Questionnaire.
One study presented data on SAS that compared 'SCS ON' with 'SCS OFF' [11], and there was a significant increase in SAS following SCS (WMD:0.65, 95% CI: [0.23,1.07], p=0.02) (Figure 6B).
Three studies reported data on SAQ [15-17] and included these five aspects: physical limitation, angina stability, angina frequency, treatment satisfaction, and disease perception. There was a significant increase when 'SCS ON' to 'SCS OFF' was compared in physical limitation (WMD: 13.09, 95% CI: [1.54, 24.64], p=0.03, test of heterogeneity: χ2=4.19, I2=52%, p=0.12), angina stability (WMD: 25.68, 95% CI: [1.47, 49.89], p=0.04, test of heterogeneity: χ2=7.65, I2=74%, p=0.02), angina frequency (WMD: 19.69, 95% CI: [0.54, 38.83], p=0.04, test of heterogeneity: χ2=4.11, I2=51%, p=0.13) and disease perception (WMD: 17.12, 95% CI: [8.05, 26.19], p=0.0002, test of heterogeneity: χ2=1.55, I2=0%, p=0.46). There was a trend towards a high level of treatment satisfaction for SCS when compared to SCS OFF (WMD: 6.24, 95% CI: [-4.12, 16.6], p=0.24, test of heterogeneity: χ2=3.84, I2=48%, p=0.15), but the result was not statistically significant (Figure 6C).
Adverse events
Three studies showed data on SCS relevant adverse events, including cerebrovascular events [10, 12] as well as total events excluding SCS/PMR related events[9]. There was no difference in cerebrovascular events when comparing 'SCS ON' to 'SCS OFF' and there seemed to be a trend towards lower cerebrovascular events in SCS when compared to CABG (OR: 0.21, 95% CI: [0.04, 1.05], p=0.06) (Figure 7A), but this trend did not yield statistical significance. There was a higher level of total events with SCS compared to PMR (OR: 3.59, 95%CI: [1.01, 12.73], p=0.05) (Figure 7B).
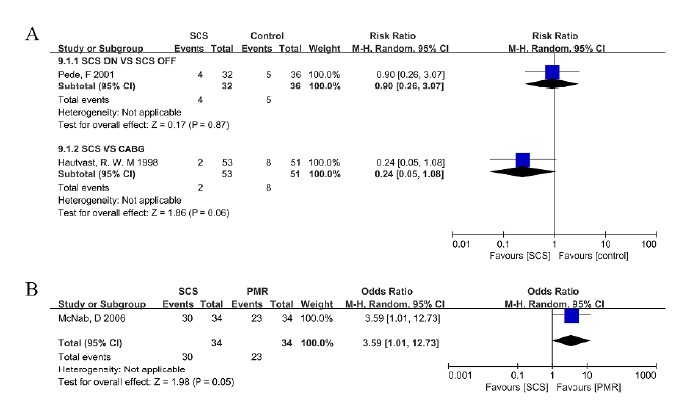
Figure 7: Forest plot of adverse events – difference among groups: A (cerebrovascular events), B (total events).
CCS class change
Two studies reported the CCS (Canadian Cardiovascular Scale) class change [16, 17], although the pooled result showed a trend towards an increase in the CCS class change (WMD: 0.76, 95%CI: [-0.02, 1.54], p=0.06, test of heterogeneity: χ2=2.2, I2=55%, p=0.14) following SCS, but it was not statistically significant (Figure 8).
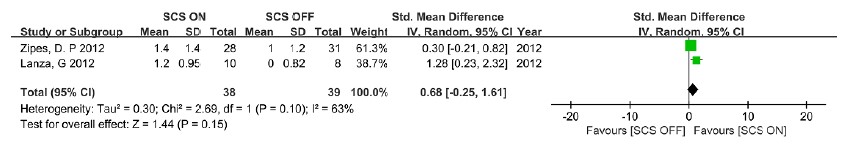
Figure 8: Forest plot of Canadian Cardiovascular Scale class change – difference among groups.
Discussion
This meta-analysis included nine studies with 364 patients diagnosed with RA. Our purpose was to compare the efficacy and safety of SCS with other treatment options. The patients' inclusion criteria were roughly similar to the following criteria: AHA III/IV or CCS class 3/4 and unsuitable for revascularization. Seven trials compared SCS with non-stimulation treatments, and the other two trials compared SCS with active-intervention treatments (CABG or PMR).
Our study revealed that SCS significantly decreased nitrate drug usage, angina attack frequency, and increased the HQROL including the social active score and SAQ (physical limitation, angina stability, angina frequency, and disease perception) when compared to 'SCS OFF' and there was a tendency to reduce the CCS class; no statistically significant difference and no difference was noted for exercise capacity and adverse events, respectively. The improvement of SCS outcome was similar to CABG or PMR, although CABG as a therapy for RA remained questionable [3]. SCS has been suggested to conceal angina symptoms, thereby increasing the risk of cerebrovascular events. However, we found that there was no significant difference in such events when 'SCS ON' was compared to 'SCS OFF', and it had less cerebrovascular events when compared to CABG. Our analysis showed there was an increased number of total events excluding SCS/PMR related to SCS when compared to PMR.
There are several hypotheses about SCS, but the mechanism remains unclear [19]. One study indicated that the beneficial effects were less likely to increase blood flow, but redistribution of local blood flow might play an important role in the improvement of myocardial ischemia [20]. Another study proposed that SCS stabilizes the intrinsic cardiac nervous system and improves cardiac function [21].
Our analysis has several limitations that are worth discussing. First, most of the included studies did not report their experimental methods, which increased the difficulty of estimating their quality of methodology and determining their risk of bias and potential effects of SCS. Second, when comparing SCS to inactive SCS, there was a shortage of data because the implantation procedure is difficult for patient blinding and the procedure may generate a placebo effect. However, sham operations cannot be performed for ethical reasons [22], making the placebo effect unavoidable. Third, small-scale trials might not achieve sufficient statistical power to detect potential clinical differences between treatments. To conquer these limitations, we pooled the results in the 'SCS ON' and 'SCS OFF' trials. Moreover, the treatment of most 'SCS ON' groups did not only use SCS but combined them with drug therapy such as nitrate drugs, and the various drug sources were not disclosed because different company products may have different efficacies that may influence final outcomes.
In summary, SCS decreased nitrate drug usage, angina attack frequency, and partially increased the HRQOL for patients with RA. The finite evidence based on the nine quality RCTs in this meta-analysis supports the 2007 ACC/AHA Grade IIb evidence classifications and Level B recommendation for SCS in RA patients [23]. Considering the relatively sparse evidence to support SCS as an alternative therapy, our study would support a wider range of applications of SCS in RA. In addition, high quality multicenter RCTs and more appropriate methods for patient recruiting are needed before SCS can be used as a routine therapy for RA.
Disclosure of Funding
This work was supported in part by NIH grants (NS094664, NS094224, DA033390, NS 072206, and HL117684), and the national natural science foundation of china (No.81400050).
Conflict Interests Disclosure
The authors have no conflicting interests to disclose.
References
- Mannheimer C, Camici P, Chester MR, Collins A, DeJongste M, Eliasson T, et al. The problem of chronic refractory angina; report from the ESC Joint Study Group on the Treatment of Refractory Angina. European heart journal. 2002;23(5):355-70. doi: 10.1053/euhj.2001.2706. PubMed PMID: 11846493.
- Mukherjee D, Bhatt DL, Roe MT, Patel V, Ellis SG. Direct myocardial revascularization and angiogenesis--how many patients might be eligible? The American journal of cardiology. 1999;84(5):598-600, a8. Epub 1999/09/11. PubMed PMID: 10482164.
- Svorkdal N. Treatment of inoperable coronary disease and refractory angina: spinal stimulators, epidurals, gene therapy, transmyocardial laser, and counterpulsation. Seminars in cardiothoracic and vascular anesthesia. 2004;8(1):43-58. Epub 2004/09/17. PubMed PMID: 15372127.
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science (New York, NY). 1965;150(3699):971-9. Epub 1965/11/19. PubMed PMID: 5320816.
- Shealy CN, Mortimer JT, Reswick JB. Electrical inhibition of pain by stimulation of the dorsal columns: preliminary clinical report. Anesthesia and analgesia. 1967;46(4):489-91. Epub 1967/07/01. PubMed PMID: 4952225.
- Mannheimer C, Augustinsson LE, Carlsson CA, Manhem K, Wilhelmsson C. Epidural spinal electrical stimulation in severe angina pectoris. British heart journal. 1988;59(1):56-61. Epub 1988/01/01. PubMed PMID: 3257701; PubMed Central PMCID: PMCPmc1277073.
- Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. European heart journal. 2013;34(38):2949-3003. Epub 2013/09/03. doi: 10.1093/eurheartj/eht296. PubMed PMID: 23996286.
- Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, et al. 2012 ACCF/AHA/ACP/AATS/ PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Journal of the American College of Cardiology. 2012;60(24):e44-e164. Epub 2012/11/28. doi: 10.1016/j. jacc.2012.07.013. PubMed PMID: 23182125.
- McNab D, Khan SN, Sharples LD, Ryan JY, Freeman C, Caine N, et al. An open label, single-centre, randomized trial of spinal cord stimulation vs. percutaneous myocardial laser revascularization in patients with refractory angina pectoris: the SPiRiT trial. European heart journal. 2006;27(9):1048-53. Epub 2006/03/24. doi: 10.1093/eurheartj/ehi827. PubMed PMID: 16554313.
- Mannheimer C, Eliasson T, Augustinsson LE, Blomstrand C, Emanuelsson H, Larsson S, et al. Electrical stimulation versus coronary artery bypass surgery in severe angina pectoris: the ESBY study. Circulation. 1998;97(12):1157-63. Epub 1998/04/16. PubMed PMID: 9537342.
- de Jongste MJ, Hautvast RW, Hillege HL, Lie KI. Efficacy of spinal cord stimulation as adjuvant therapy for intractable angina pectoris: a prospective, randomized clinical study. Working Group on Neurocardiology. Journal of the American College of Cardiology. 1994;23(7):1592-7. Epub 1994/06/01. PubMed PMID: 8195519.
- Di Pede F, Zuin G, Giada F, Pinato G, Turiano G, Bevilacqua M, et al. Long-term effects of spinal cord stimulation on myocardial ischemia and heart rate variability: results of a 48-hour ambulatory electrocardiographic monitoring. Italian heart journal : official journal of the Italian Federation of Cardiology. 2001;2(9):690-5. Epub 2001/10/23. PubMed PMID: 11666098.
- de Jongste MJ, Staal MJ. Preliminary results of a randomized study on the clinical efficacy of spinal cord stimulation for refractory severe angina pectoris. Acta neurochirurgica Supplementum. 1993;58:161-4. Epub 1993/01/01. PubMed PMID: 8109281.
- Hautvast RW, DeJongste MJ, Staal MJ, van Gilst WH, Lie KI. Spinal cord stimulation in chronic intractable angina pectoris: a randomized, controlled efficacy study. American heart journal. 1998;136(6):1114-20. Epub 1998/12/08. PubMed PMID: 9842028.
- Eddicks S, Maier-Hauff K, Schenk M, Muller A, Baumann G, Theres H. Thoracic spinal cord stimulation improves functional status and relieves symptoms in patients with refractory angina pectoris: the first place-bo-controlled randomised study. Heart. 2007;93(5):585-90. doi: 10.1136/hrt.2006.100784. PubMed PMID: 17237126; PubMed Central PMCID: PMC1955532.
- Lanza GA, Grimaldi R, Greco S, Ghio S, Sarullo F, Zuin G, et al. Spinal cord stimulation for the treatment of refractory angina pectoris: a multicenter randomized single-blind study (the SCS-ITA trial). Pain. 2011;152(1):4552. doi: 10.1016/j.pain.2010.08.044. PubMed PMID: 21084162.
- Zipes DP, Svorkdal N, Berman D, Boortz-Marx R, Henry T, Lerman A, et al. Spinal cord stimulation therapy for patients with refractory angina who are not candidates for revascularization. Neuromodulation : journal of the International Neuromodulation Society. 2012;15(6):550-8; discussion 8-9. doi: 10.1111/j.1525-1403.2012.00452.x. PubMed PMID: 22494013.
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC medical research methodology. 2005;5:13. doi: 10.1186/1471-2288-5-13. PubMed PMID: 15840177; PubMed Central PMCID: PMC1097734.
- Ekre O, Eliasson T, Norrsell H, Wahrborg P, Mannheimer C. Long-term effects of spinal cord stimulation and coronary artery bypass grafting on quality of life and survival in the ESBY study. European heart journal. 2002;23(24):1938-45. Epub 2002/12/11. PubMed PMID: 12473256.
- de Vries J, Foreman RD, DeJongste MJ. The anti-ischemic effects of electrical neurostimulation in the heart. Cleveland Clinic journal of medicine. 2007;74 Suppl 1:S42-7. Epub 2007/04/26. PubMed PMID: 17455543.
- Cardinal R, Page P, Vermeulen M, Bouchard C, Ardell JL, Foreman RD, et al. Spinal cord stimulation suppresses bradycardias and atrial tachyarrhythmias induced by mediastinal nerve stimulation in dogs. American journal of physiology Regulatory, integrative and comparative physiology. 2006;291(5):R1369-75. Epub 2006/06/17. doi: 10.1152/ajpregu.00056.2006. PubMed PMID: 16778070.
- Van Zundert J. Clinical research in interventional pain management techniques: the clinician's point of view. Pain practice : the official journal of World Institute of Pain. 2007;7(3):221-9. Epub 2007/08/24. doi: 10.1111/j.1533-2500.2007.00139.x. PubMed PMID: 17714100.
- Fraker TD, Jr., Fihn SD, Gibbons RJ, Abrams J, Chatterjee K, Daley J, et al. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. Journal of the American College of Cardiology. 2007;50(23):2264-74. Epub 2007/12/07. doi: 10.1016/j.jacc.2007.08.002. PubMed PMID: 18061078.