Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/083
SPECIAL REPORTOPEN ACCESS
The Stroke Prehospital Delay Summary Statement: A Global Battlefield
Jing Zhao, MD, PhD#,1, Lijie Ren, MD, PhD#,2, Siju V Abraham, MD3, Dou Li, MD, PhD4, David Kung, MD5, A-Ching Chao, MD, PhD6, Marc Fisher, MD7, Renyu Liu, MD, PhD*,8,1
#Contributed as co-first authors
1Department of Neurology, Minhang Hospital, Fudan University, Shanghai, China
2Department of Neurology,The First Affiliated Hospital of Shenzhen University, Shenzhen Second People's Hospital, Shenzhen, China
3Department of Emergency Medicine, Jubilee Mission Hospital, Medical College & Research Institute, Kerala, India
4Beijing Emergency Medical Center, Beijing, China
5Department of Neurosurgery, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, USA
6Department of Neurology, Kaohsiung Medical University & Hospital, Kaohsiung, Taiwan
7Department of Neurology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, USA
8Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, USA
Renyu Liu, MD; PhD, Associate Professor, Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania; Director of Stroke 120 Special Task Force, Chinese Stroke Association, Center of Penn Global Health Scholar; 336 John Morgan Building, 3620 Hamilton Walk, Philadelphia, PA 19104, USA, E-mail: liur@uphs.upenn.edu
Editor: Henry Liu, MD, MS, FASA, Professor of Anesthesiology, Vice Chairman for Research, Drexel University College of Medicine, Hahnemann University Hospital, 245 N. 15th Street, MS 310, Philadelphia, PA 19102, USA, E-mail: henryliupa@gmail.com
Received: January 14, 2019 | Accepted: January 21, 2019| Published: January 29, 2019
Citation: Zhao J, Ren L, Abraham SV, Li D, Kung D, Chao A-Ching, Fisher M, Liu R. The Stroke Prehospital Delay Summary Statement: A Global Battlefield. Transl Perioper & Pain Med 2019; 6 (1):20-26.
Abstract
An international symposium specifically focusing on prehospital delay and potential strategies to reduce prehospital delay for stroke was held in the Penn Wharton China Center on June 28th, 2018 in Beijing. More than 70 experts from across China and other countries and regions attended this symposium, which was streamed live across China. There were 11,318 active participants online during the symposium, indicating enormous enthusiasm for this topic. Prehospital delay for stroke patients is a critical global issue. It should be considered as a crisis in many developing countries and regions, requiring immediate implementation of practical strategies to reduce prehospital delay. The symposium focusing on prehospital delay for stroke patients generated very productive discussions on the causes of long prehospital delays, including poor public awareness and poor willingness to utilize emergency medical systems. Potential solutions and strategies discussed include the use of novel educational tools (Stroke 120 and Stroke 112, both of which are based on FAST: Face, Arm, Speech, Time) to improve awareness and emergency medical system utilization, establishment of robust emergency stroke care systems and stroke care maps, and an enhancement in governmental support etc. Removal of informed consent for thrombolytic therapy in some countries and regions was strongly recommended. As most of the proposed solutions are from expert opinions, future efforts could focus on testing these strategies and proposing new recommendations or guidelines for this specific important global health issue.
Keywords
Stroke, Prehospital delay, Education, Strategy
Stroke remains a leading cause of death and disability worldwide, ranked second after cardiac disease [1]. Ischemic stroke accounts for approximately 80% of all stroke events. While recombinant tissue plasminogen activator (tPA) and thrombectomy are available for ischemic stroke, the use of thrombolytic therapy remains very low (< 10%) in many countries and regions worldwide, with long prehospital delay time cited as one of the major causes [2,3]. We reviewed available data from India, China, Japan, and Korea, where the median or mean prehospital delay time range from 11 to 20 hours, even in urban areas [2-4]. Inclusion of suburban areas would make the prehospital delay time even worse in these nations. Based on these considerations, prehospital delay should be considered as a global crisis, especially in less developed and non-English speaking countries and regions. Such long prehospital delay time is largely due to poor public awareness, poor usage of existing emergency medical systems (EMS), or lack of EMS itself. These obstacles need to be addressed, and novel effective strategies are needed to reduce prehospital delay time in these areas. An international symposium specifically focusing on prehospital delay and potential strategies was held in the Penn Wharton China Center on June 28th, 2018. More than 70 experts from across China and other countries and regions attended this symposium, which was streamed live across China. 11,318 active participants were online during the symposium, indicating enthusiasm for this topic.
The following factors affecting prehospital delay for stroke were discussed
Poor Public Awareness
Awareness of stroke is poor across the world, especially in developing countries, and this poor awareness is also evident amongst non-neurologists and family physicians [2,4-6]. Professor John Zhang, the Editor in Chief of Translational Stroke Research, from Loma Linda University, offered an example of a United States medical school professor who failed to realize he had suffered a stroke, urging strengthening education in public awareness of stroke and stroke recognition. The lack of an effective awareness/educational tool has been well documented. Dr. A-Ching Chao, the secretary general of the Taiwan Stroke Research and Therapy Society, pointed out that although FAST (Face, Arm, Speech, and Time) has been used in Taiwan for many years, its effectiveness is very poor due to linguistic barriers. While many strategies have been tried in the past few years, none have shown optimal effectiveness.
Poor Willingness to Trigger EMS by calling an Emergency Phone Number
Dr. Li, the president of the Society of Emergency Medicine of the Chinese Stroke Association, pointed out that the poor awareness in using EMS was one of the major factors in prolonging prehospital delays for stroke patients in China. Less than 15% of people in India use EMS, as pointed by Dr. Siju V. Abraham, an emergency physician from India. Even in some well-developed countries, the use of EMS remains below 60%. A study from the US investigated a nationally representative sample of emergency visits for stroke patients between 2003-2009 found that EMS usage remained around 50% [7].
Poor EMS
In some developing countries, EMS is not well developed. Dr. Siju V Abraham stated that there are a very limited number of operational ambulances in India that actually provide prehospital care. Most of the existing ambulances are run by different entities associated with various different emergency numbers [4]. There are no trained personnel, nor is there an accredited EMS training program endorsed by the Medical Council of India as of now in the country. Most of the ambulances are run solely for transport without any needed medical management. Although the Indian government has been trying to implement a unified international emergency phone number (112) since 2017, it is not yet well implemented ( https://indianexpress.com/article/india/112-to-become-indias-new-emergency-number, accessed on August 8, 2018). In remote areas of many countries, EMS is not well developed and does not have enough ambulances. Therefore, it may take too long for an ambulance to be dispatched or to reach patients.
Inconsistent Emergency Phone Numbers
While 120 is the specific emergency medical phone number in China [3], many hospitals use an emergency phone number unique to their hospitals. Such numbers could be as long as 11 digits (Figure 1). It is difficult for people to remember such long numbers, and more numbers could cause more dialing mistakes and further delays. While this advertisement in figure 1 educates people where and how to get ischemic stroke treatment, it is doubtful whether anyone could remember such a long emergency phone number while quickly passing by this advertisement along the highway.
Figure 1: An advertisement for stroke management on the side of the highway. The portion outlined in red indicates the 11 digits of the emergency phone number. It is not an uncommon practice in China for many local hospitals to have their own specific emergency phone numbers, even though 120 as a standard specific medical emergency phone number has been implemented for many years.

Poor knowledge of which hospitals have appropriate stroke management capabilities
In many areas in China and around the world, it is unclear which hospitals have stroke management capabilities. This is especially true in rural areas, where many hospitals have no stroke treatment center or specialized stroke management capabilities. Some patients need to be re-transferred to hospitals that have the stroke management capabilities, causing further delay in accessing thrombolytic therapy due to transfer procedures and additional travel.
Inability to diagnose stroke in a timely manner, especially patients with major vessel occlusion needing thrombectomy
It is evident that the knowledge to identify potential stroke patients, especially patients with potential large vessel occlusions, is very poor.
Poor traffic conditions
While there are many stroke centers in urban areas with robust EMS, congested traffic conditions are another critical factor in prehospital delay.
Inadequate government support
Since prehospital education is generally not considered a critical academic mission, research funding allocation from government is very limited in many countries. It is the government's responsibility to establish a robust EMS and make proper educational programs available. However, EMS is not well-developed in many countries and regions, especially in developing countries. Educational programs are not well-developed.
Unclear responsibilities
There are unclear responsibilities regarding who should be responsible for prehospital education. Prehospital effort is mistakenly considered as a non-academic activity, merely considered as public education not associated with high level outcome improvement.
The requirement for consent for thrombolytic therapy in some countries and regions
Both in China and India, informed consent for thrombolytic therapy is needed, adding additional delay to the time-sensitive therapy.
The following potential solutions were discussed:
Novel stroke awareness programs are needed, especially in non-English speaking countries and regions. Such a program should be easily remembered without language barriers and not require higher education to understand. All the experts attending the symposium agreed that Stroke 1203 fits these criteria well and should be used for stroke awareness and education in China. During the past 2 years, Stroke 120 has been widely accepted and promoted across China, as pointed out by Dr. Yuming Xu, the president of the Henan Stroke Society. In other non-English speaking countries and regions where 112 is used as the emergency phone number, Stroke 112 as a simple educational tool was discussed.2 Dr. A-Ching Chao, who said that Stroke 112 is well-accepted in Taiwan and it plays a critical role in stroke education there, said "Our society uses this novel tool to educate people in the public domain, to have direct linkage for those with stroke symptoms to trigger EMS immediately, shortening decision making time." Dr. Zhouqin Feng, a senior neurologist from Henan Province, commented that without the initiation of the emergency phone call after rapid recognition/identification of a stroke episode the usefulness of novel technology including a mobile stroke unit will be very limited.
It is critical to educate people that only through ambulance transport can stroke patients enter a stroke fast care track, therefore avoiding waiting in the emergency room and reducing in-hospital delays.
It is critical to avoid medical jargon in public education.
We used to think that our mission was to educate patients. However, we now realize that it is not enough to simply educate patients, but the public as well. It is critical to educate the young generation, who are likely to make the decision to seek medical treatment for their elderly family members. Dr. Qingfeng Ma from Xuanwu Hospital, urged that we educate everyone and noted that different strategies are needed in targeting individuals with different backgrounds and ages. This educational effort is a long term task needing efforts from many generations One of the experts proposed the incorporation of an educational program in school systems and said that stroke awareness education should also be part of the required component for continued medical education across all subspecialties. All members of society should be able to recognize the signs and symptoms of stroke and call an emergency phone number if someone is having a stroke.
Educating community hospital physicians and family doctors is critical, and they should be trained as key members of the stroke care team. Dr. Wenzhi Wang from Beijing pointed out that, based on his research, educational programs targeting communities and community hospital physicians could improve ambulance usage when a stroke is suspected.
Educating EMS staff and operators/dispatchers in the EMS center was also discussed. Operators/dispatchers in the EMS center could help to identify potential stroke patients and prioritize ambulance dispatch for stroke patients. EMS staff should improve their knowledge to identify stroke patients on site, perform the Cincinnati Prehospital Stroke Scale (CPSS) or National Institute Stroke Scale (NIHSS) evaluation, helping them to make a preliminary diagnosis for stroke. It is critical to identify potential major vessel occlusion based on the stroke scale by EMS staff on site. Since there are far fewer facilities having the capability to perform thrombectomy, it is critical that paramedics, primary-care physicians, and even individuals in the public domain have the capability to identify stroke patients with potential large vessel occlusion as soon as possible. The patient could potentially be transferred to proper stroke centers immediately to avoid delay associated with re-transfer.
In addition to the prehospital education program, an in-hospital education program should be developed since stroke patients are at risk for recurrence. Some subsequent stroke events are much more severe than the first stroke, with much higher mortality and disability rates. Hospital settings provide a great opportunity and resources to teach patient and family members. It is possible that the effectiveness of education could be much higher in the hospital settings. Dr. Marc Fisher, the Chief Editor of Stroke, introduced that he generally teaches his stroke patient: "You must understand the symptoms of a stroke. A second stroke is a real possibility. You should plan for it so that you can come to the hospital and treat it faster when you have a stroke again. I think all doctors should also teach this to their patients."
The training of the specialized stroke educator is needed as proposed by Dr. Kunwen Zheng, an outstanding stroke educator from Yunnan Province. The specialized stroke educator should have the following requirements:
● Professionalism with scientific rigors
● Use standardized language yet easy to understand
● The capability to deliver professional knowledge into ordinary people's life knowledge.
● Be passionate, fun, and interesting.
A stroke educational camp was proposed and discussed by Dr. Lei Xia. Such a camp is very helpful in training physicians from community hospitals. Such training is very effective and generally includes an in-training exam. Attendees agreed that such training camps should be implemented nationwide. Establishing special task forces targeting prehospital delay lead by neurologists is an effective way to mobilize regional resource to educate the public, as described by Dr. Guozhong Li, the director of the Stroke 120 Heilongjiang Special Task Force.
Removal of informed consent for thrombolytic therapy was discussed. While informed consent for thrombolytic therapy is not required in some countries, it is needed in many countries and regions. China is one of the countries that requires informed consent for thrombolytic therapy, adding further delay in accessing the critical therapy to re-establish blood flow to the ischemic brain region. In some cases, consent is denied by the family members due to lack of understanding or fear of side effects. The proposal to remove informed consent was echoed by attendees of the symposium with extensive support. Dr. Marc Fisher strongly urged that the stroke societies should work closely with the governments to eliminate informed consent for thrombolytic therapy. However, Dr. Siju V Abraham from India commented: "Informed consent is not something we in India can avoid for two reasons: 1) Cost of the drug, 2) The drug still has a side effect profile that we need to worry about".
The role of maps showing hospitals or centers that have stroke care capabilities was discussed. This topic was initiated by Dr. Lijie Ren, the creator of the Thrombolysis Map (currently knows as Stroke Emergency Map) in China. The Thrombolysis Map is supported by local healthcare administrations and was merged into the complete acute stroke activation protocol, which consists of EMS personnel training, ambulance dispatch and triage guideline, and stroke center standard. The map unites all the qualified local hospitals or centers that can provide intravenous thrombolysis and/or endovascular thrombectomy. EMS work seamlessly with these hospitals to optimize stroke care systematically. The availability of such map should guide the EMS to send the stroke victims to a nearby hospital that has the suitable stroke care capabilities. It could serve other functions such as:
● Guiding policy makers to establish new stroke centers in areas that are under-served.
● Promoting the awareness of nearby hospitals with stroke care capabilities. The patient and family members have the right to discuss with the EMS staff which hospital the stroke victim will be sent to (legal responsibility and transparency to avoid unethical, financially driven behaviors)
● Reducing both prehospital and in-hospital delay (the onset-to-needle time, ONT)
● Promoting the establishment and improvement of the pre-hospital emergency network
● Promoting improvement in the quality of stroke centers
● Promoting the formation of a stroke referral system.
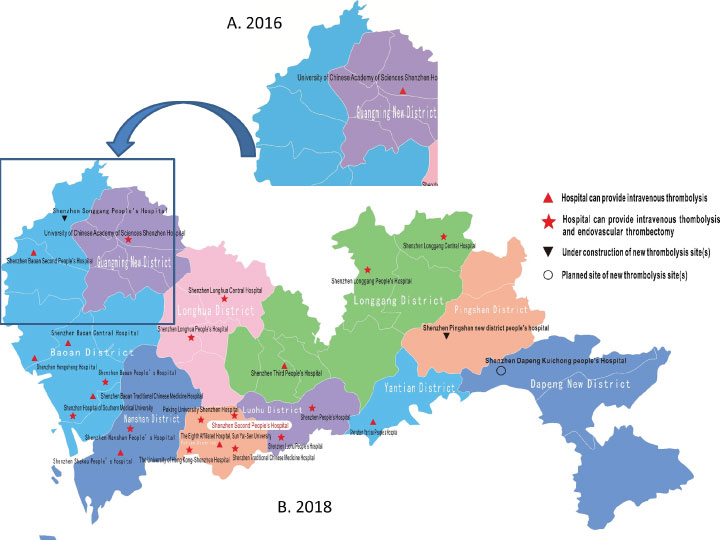
Such thrombolysis maps have been established in multiple areas in China with a positive outcome to increase the thrombolysis rate. Figure 2 demonstrates the development of the first Stroke Emergency Maps established in Shenzheng that was initiated by Dr. Ren. Part of the 2016 version of this map is presented in Figure 2A and clearly indicates areas that lack stroke care resources. Efforts were taken to increase the number of sites in the under-served areas indicated in this figure. In the new 2018 version of the map (Figure 2B), centers that have thrombectomy capabilities are clearly indicated and sites undergoing construction or planned are also indicated. There is an official certification process for the approval for these sites. The new site of Shenzhen Baoan Second People's hospital noted in the square window in Figure 2, although it is not certified for thrombectomy yet, the service has started with the guidance of the experts from certified centers.
Figure 2: Stroke Emergency Care Map of Shenzhen. Panel A shows part of the very first map released. The map shows an area with high population density that has only one facility with capability for thrombolysis. Panel B is the updated version of the map for 2018. New sites are established or under construction to improve regional accessibilities of stroke care. The map also clearly indicates which facilities have thrombectomy capabilities. The initial map served as important tool to guide policy makers and hospitals to establish new sites for the under-served area. A Red "▲"indicates hospitals that have stroke care capabilities. Red "★" indicates hospitals that have both capabilities. Black "▼"indicates a new site under construction. "○" indicates a new planned site.
The benefits of telemedicine in reducing prehospital delay were discussed. Multiple experts commented that telemedicine could guide accurate evaluation of the patient on-site, perform initial NIHSS or CPSS evaluation, and alert the stroke center as early as possible to get ready to reduce in-hospital delay. Such telemedicine is very useful in rural and remote locations. Telemedicine could also help to identify stroke patients who might have large vessel occlusion, guide patient management during transportation, etc.
The role of the government in reducing prehospital delay was also discussed. Mr. Baohua Chao, the Director of the Secretariat of Stroke Prevention Project of National Health Commission of the People's Republic of China, discussed that the Chinese government should and will play a critical role in education and reducing prehospital delay through the following strategies:
● Strengthen educational programs with a persistent long-term program approach.
● Enhance the stroke emergency network establishment.
● Establish more centers with stroke care capabilities.
● Strengthen the stroke fast track (Green Channel) in more hospitals. Enhance training, especially the training for the physicians in the community hospitals.
● Establish a system for easy access to stroke care. For example, authorizing treatment before payment authorization.
● Enhance government monitoring to improve stroke care quality etc.
Dr. Siju V Abraham suggested that the government should consider helping stroke patients pay for thrombolytic medication cost or part of the total cost of the therapy if the stroke patient arrives at the hospital within 2 hours to encourage patients to reach the hospital as quickly as possible. Legislative changes warranting timely and appropriate referral of patients to officially-certified stroke care centers would prevent stagnation of the stroke patients at primary care centers. Legislative regulations by the government were discussed. Dr. David Kung from the University of Pennsylvania Stroke Center said that there is no legislation in dealing with prehospital delay for stroke victims in the United States. Stroke patients requiring transfer could potentially bypass a closer tertiary stroke center due to hospital and insurance affiliations, adding time delay in treatment. Guidelines are being developed but local practices vary significantly. In countries and areas where EMS is not well established, it is critical to use a standardized medical emergency phone number. 112 is the standard international emergency phone number, and it should be adopted for those countries and regions where there are no consistent emergency phone number. It is the government's responsibility to adopt legal regulations or at least moral regulations to avoid using internal medical emergency phone numbers for financial gain. Corruption in EMS should also be monitored and regulated. A violation by sending stroke patients to remote hospitals bypassing nearby hospitals with stroke management capabilities without proper medical reasons should be punished. The insurance company should encourage and reimburse medical costs if the stroke victims are sent to the nearby hospitals that have no financial contract with the specific hospitals. Prehospital stroke education is a critical academic activity. Vigorous research programs should be initiated with resources and funding support from the government, society, and other related funding agencies. "Prehospital delay is certainly a critical global issue. Our society and I are eager to work with experts from across the world to solve this through implementing public education and research," said Dr. Han-Hwa Hu, the president of the Taiwan Stroke Research and Therapy Society, from Taipei Medical University.
In summary, prehospital delay for stroke patients is a critical global issue. It should be considered as a crisis in many developing countries and regions due to long prehospital delay, needing immediate implementation of practical strategies to reduce the delay. The symposium focusing on prehospital delay for stroke patients offered very productive discussions on the causes of long prehospital delays, including poor public awareness, poor willingness to utilize EMS, etc. The potential solutions and strategies include novel educational tools (Stroke 120 and Stroke 112) to improve awareness, improve EMS utilization, establish robust EMS with a region-specific stroke care system and stroke care map, increase governmental support etc. While most of the proposed solutions are from expert opinions, future effort could focus on testing these strategies and proposing new recommendations or guidelines for this specific important medical issue.
Acknowledgements
In addition to the experts mentioned in the summary, we also thank the following experts who contributed their precious time and effort to participate in this symposium and offered meaningful discussion and opinions. Zhuo Zhang (Chinese Stroke Association), Jinai He (Jinan University), John Zhang (University of Pennsylvania), Huisheng Chen (Liaoning Neurological Disease Research Center), Guangjian Zhao (Shangdong), Tao Chen (Kunming University), Hongliang Huo (Capital University), Kaifu Ke (Nantong University), Xiaoyuan Niu (Sichuang University), Temuqile (Inner Mogolia University); Shudong Qiao (Capital Steel Hospital), etc. The authors would like to thank the research team in Dr. Lijie Ren'd department for assisting the Shenzhen 2018 version of the thrombolysis map. The authors appreciate the editing assistance from Amey Vrudhula at the department of Anesthesiology and Critical Care at the University of Pennsylvania.
Funding
We appreciate the following funding support from the National Natural Science Foundation of China (81572232, PI: JZ); Shanghai Natural Science Foundation (17dz2308400, PI: JZ). China Research Engagement Funding from the University of Pennsylvania (PI, RL).
Science and Technology Innovation program of Shenzhen Science and Technology Commission (No.KJYY20180703165202011, PI:LR);Shenzhen health and population family planning commission (No.SZLY2017012, PI:LR).
Financial Disclosure
No conflict of interests for any of the authors of this manuscript.
Endorsement
This consensus received endorsements from the following organizations: 1) Society of the Emergency Medicine of the Chinese Stroke Association, 2) the Stroke 120 special task force of the Chinese Stroke Association, 3) the Taiwan Stroke Research and Therapy Society (STARS-Taiwan); 4) Emergency Medicine Association India.
References
- Sarti C, Rastenyte D, Cepaitis Z, Tuomilehto J. International trends in mortality from stroke, 1968 to 1994. Stroke. 2000; 31:1588-1601.
- Zhao J, Eckenhoff MF, Sun WZ, Liu R. Stroke 112: A universal stroke awareness program to reduce language and response barriers. Stroke. 2018; 49:1766-1769.
- Zhao J, Liu R. Stroke 1-2-0: A rapid response programme for stroke in china. Lancet Neurol. 2017; 16:27-28.
- Abraham SV, Krishnan SV, Thaha F, Balakrishnan JM, Thomas T, Palatty BU. Factors delaying management of acute stroke: An indian scenario. Int J Crit Illn Inj Sci. 2017; 7:224-230.
- Farrag MA, Oraby MI, Ghali AA, Ragab OA, Nasreldein A, Shehata GA, et al. Public stroke knowledge, awareness, and response to acute stroke: Multi-center study from 4 egyptian governorates. J Neurol Sci. 2018; 384:46-49.
- Kim YS, Park SS, Bae HJ, Heo JH, Kwon SU, Lee BC, et al. Public awareness of stroke in korea: A population-based national survey. Stroke. 2012; 43:1146-1149.
- Tataris K, Kivlehan S, Govindarajan P. National trends in the utilization of emergency medical services for acute myocardial infarction and stroke. West J Emerg Med. 2014; 15:744-748.