Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/087
REVIEW ARTICLE OPEN ACCESS
Post Thoracic Surgery Pain Management: A Novel Regional Approach beyond Epidural Catheter?
David Li, MD, Aubrey Yao, MD and Hong Liu, MD, FASE*
Department of Anesthesiology and Pain Medicine, University of California Davis Health, Sacramento, California, USA
Hong Liu, MD, FASE, Professor, Department of Anesthesiology and Pain Medicine, University of California Davis Health, 4150 V Street, Suite 1200, Sacramento, CA 95817, USA, Tel: 916-734-5031, Fax: 916-734-7980, E-mail: hualiu@ucdavis.edu
Editor: Tianzuo Li, MD, PhD, Professor, Department of Anesthesiology, Beijing Shijitan Hospital affiliated to Capital Medical University, Beijing, China, E-mail: trmzltz@126.com
Received: February 09, 2019 | Accepted: February 27, 2019| Published: February 28, 2019
Citation: Li D, Yao A, Liu H. Post Thoracic Surgery Pain Management: A Novel Regional Approach beyond Epidural Catheter?. Transl Perioper & Pain Med 2019; 6 (2):49-52.
Perioperative care of the thoracic surgery patient is often focused on lung isolation, management of hypoxemia, and avoidance of acute lung injury. In the context of these acute needs, postoperative analgesia frequently becomes an afterthought. However, poor postoperative pain control significantly delays a patient's recovery, increases postoperative morbidity, and even leads to increased healthcare costs [1]. Excessive reliance on opioid-based analgesia can result in nausea, vomiting, ileus, respiratory depression and oversedation. Therefore, there is a significant need for improved postoperative analgesic regimens for thoracic surgery patients.
Until recently, thoracic epidurals and thoracic paravertebral blocks have been the primary analgesic alternatives for thoracic surgical patients. However, the increasing complexity of thoracic surgical procedures coupled with the extensive utilization of systemic anticoagulants and antiplatelet medications have limited the widespread adoption of these neuraxial and regional anesthetic techniques. The erector spinae plane (ESP) block was first introduced in 2016 for the treatment of thoracic neuropathic pain. Since that time, it has shown great potential as an alternative regional anesthetic technique for thoracic surgery [2].
At our institution, we have incorporated the ESP block for some of our complex thoracic surgical patients. As an example, a 75-year-old man presented for a right thoracotomy and bilobectomy of the middle and lower lobes for squamous cell carcinoma. The right lower lobe mass measured 13.4 cm × 9.4 cm, with involvement of the mediastinum, diaphragm, and mass effect on the right atrium. The surgical plan involved an open thoracotomy with cardiopulmonary bypass (CPB) standby in the event of intractable surgical bleeding. Since emergent CPB would require full heparinization, a thoracic epidural was not placed preoperatively. Alternatively, after discussion with the thoracic surgeon, a right-sided ESP catheter (for use postoperatively) was placed preoperatively.
This patient had an uneventful intraoperative course without the need for emergent CPB. A total of 600 mcg of intravenous (IV) fentanyl and 0.4 mg of IV hydromorphone was administered during a 7.5 hour long operation. The ESP catheter infusion was initiated postoperatively with 0.1% ropivacaine at 12 mL/hour. The patient was also given an IV hydromorphone patient-controlled analgesia (PCA) for breakthrough pain. On postoperative day (POD) one, he reported a 0 out of 10 on the verbal pain score at rest and with movement. He also demonstrated a reliable sensory block from T5 to T10 in the anterolateral thorax region. On POD 2, the ESP catheter infusion rate was decreased to 10 mL per hour and the patient continued to report a 0 out of 10 pain severity with no additional requirement for PCA or other rescue opioid adjuncts. On POD 3, the ESP block catheter was removed with patient able to get out of bed and ambulate with minimal pain. The patient's hospital course was uneventful, with discharge to home without any major postoperative complication.
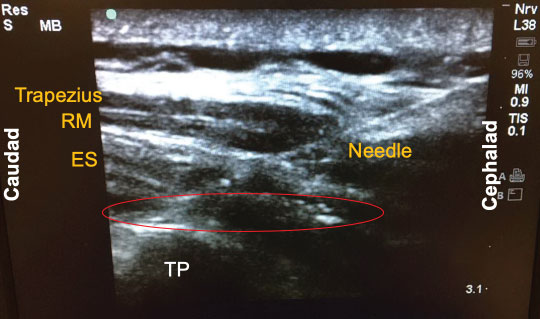
Since its introduction a few years ago, there have been numerous descriptions published on how to perform the ESP block. The following is a brief summary of the technique used to perform the block on our previously-described patient. With the patient in the sitting position, a high-frequency linear ultrasound probe was placed longitudinally on the patient's back approximately 3 cm lateral to the 5th thoracic (T5) spinous process. Three muscles above the hyperechoic transverse process were identified: trapezius, rhomboid major, and erector spinae in order of superficial to deep layers (Figure 1). A 10-cm 18-gauge Tuohy needle was inserted in-plane with the ultrasound beam at a 30° angle in a cephalad to caudal fashion. The tip of the needle was directed to the myofascial plane between the erector spinae muscle and the T5 transverse process (Figure 2). Following negative aspiration of blood, 20 mL of 0.25% ropivacaine was incrementally injected. Linear fluid spread deep to the erector spinae muscle was visualized in real-time. Finally, for continuous postoperative infusion, a 20-gauge catheter was threaded through the Tuohy needle and secured at the skin with a goal of having 5 cm of catheter left in the myofascial plane.
Figure 1: Three muscle layers for the erector spinae plane (ESP) block: Trapezius, rhomboid major (RM), and erector spinae (ES).
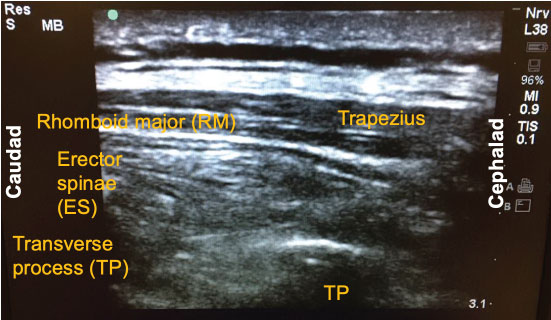
Figure 2: Local injection into the erector spinae (ES) plane. The tip of the needle (red circle) was directed to the myofascial plane between the erector spinae muscle and the T5 transverse process (TP). RM: Rhomboid Major.
The exact mechanism of action of the ESP block has yet to be fully delineated. However, it has been postulated that the local anesthetic injected via the ESP block around the T5 region results in both somatic and visceral analgesia of T2 to T9 sensory level by blocking both dorsal and ventral rami of spinal nerves, including the sympathetic chain [2]. Similarly, in our case scenario above, the patient had a reliable sensory block from T5 to T10 anterolateral thorax region on POD 1. This case also highlighted some of the advantages of this novel regional technique: Minimally invasive, relatively easy to perform, provides good sensory coverage for various thoracic surgical procedures, and safe with a low complication rate. Variations of target entry sites for the ESP block with different dermatomal coverage have been documented in the literature, ranging from high thoracic (T2) to low lumbar (L4) [3]. The variability of the block's entry site and potential clinical application is likely due to tissue plane block nature of this regional technique and the interindividual variability in the extent of the spread of the local anesthetic. This point is supported by the variable craniocaudal spread of dye (C7 to T8) observed in a cadaver study involving injections into the erector spinae plane [2]. Given all these unclear factors, are there actual data supporting these claims and the mainstream adaptation of the ESP block for thoracic surgical patients?
Since the ESP block is a relatively new regional anesthesia technique, there is a paucity of well-designed randomized controlled trials investigating its efficacy compared to other more invasive techniques. One recent prospective randomized controlled trial evaluated bilateral ESP block for acute postsurgical pain in 116 patients undergoing elective cardiac surgery. The authors found that patients in the ESP block group had a significantly higher mean duration of analgesia, defined as patients with a pain numeric rating scale < 4 out of 10, compared with the control group [4]. In addition, they found that the ESP group had reduced perioperative total opioid usage, and no other adverse events (such as bleeding and hematoma formation). Similarly, another group has demonstrated the benefits of utilizing continuous bilateral ESP block catheters to enhance the recovery process for patients undergoing elective open cardiac surgery [5]. Their study showed the ESP block group received significantly reduced amount of opioid both intraoperatively and 48 hours postoperatively, therefore promoting faster recovery in the postoperative period. These data can likely be applied to thoracic surgical patients as well, given their similarities in comorbidities and the invasive natures of the both types of surgery.
In a review of 85 publications with 242 cases between 2016 and 2018, the authors found that the majority of the authors used single shot techniques (80.2%), followed by intermittent boluses (12.0%) and continuous infusions (7.9%) [4]. Bupivacaine and ropivacaine were the primary local anesthetics being used for these blocks, with 0.25% bupivacaine being the most commonly used followed by 0.5% ropivacaine. Local anesthetic volumes administered in the single shot technique ranged from 10-30 mL [6]. Overall, a reduction in opioid use was reported in 76.0% of cases, with 34.7% reporting sensory changes from the ESP block [6]. Equally important, there were no side effects (such as bleeding or hemodynamic instability) reported.
Effective opioid-sparing postoperative analgesia in thoracic surgery patients plays a critical role in patient recovery by promoting early mobilization, effective pulmonary hygiene, and by limiting the occurrence of major opioid side effects (ileus, vomiting, sedation, respiratory depression). Utilization of regional analgesia techniques, such as thoracic epidurals and thoracic paravertebral blocks, have decreased due to the possibility of significant complications such as persistent hypotension, pneumothorax, dural puncture, epidural hematoma, and spinal cord injury [1,7]. These invasive techniques are also relatively complex to perform and can have a failure rate as high as 15% [8]. In comparison to the thoracic epidural, ESP block provides extensive cranial-caudal spread and better coverage of multiple dermatomes with a single injection of local anesthetic [9,10]. As it is an ultrasound-guided procedure with an easily visualized target site of injection, the ESP block can be considered a simpler alternative to thoracic epidural and paravertebral block. Also, since the needle and anatomic target are farther away from vital structures such as the pleura, neuroaxis, and major vasculature, the ESP block is safer to perform with less chance of major complication [2].
In summary, the ESP block has the potential to provide excellent analgesia for a good duration in thoracic surgery patients compared with other more invasive neuraxial techniques or IV only regimens. Its utility in specific thoracic surgical procedures and specific patient populations remains to be further delineated in future studies. But the relative simplicity and safety of the ESP block confers the potential to be a useful regional intervention in wide range of clinical scenarios such as rib fractures [11], failed thoracic epidural, and rescue analgesia for patients undergoing invasive thoracic surgeries where conventional analgesia therapies are not ideal or feasible. However, the ESP block should not be viewed as an analgesic panacea for thoracic surgical patients given its various limitations. The wide variability of local anesthetic spread due to the nature of tissue plane block still presents the problem of interindividual variability in its clinical efficacy. The placement of bilateral ESP block with catheters prior to surgery may also present a significant efficiency limitation for the surgical team and the operating room workflow. Lastly, there are no specific guidelines for anticoagulation and the ESP block; this warrants additional investigation and study. For now, we are optimistic that the ESP block will continue to play an increasingly important role as a part of the enhanced recovery after surgery protocol in adult thoracic surgical patients.
Funding Sources
This work was supported by the University of California Davis Health Department of Anesthesiology and Pain Medicine, and NIH grant UL1 TR001860 of the University of California Davis Health.
References
- Rodriguez-aldrete D, Candiotti KA, Janakiraman R, Rodriguez-blanco YF. Trends and New Evidence in the Management of Acute and Chronic Post-Thoracotomy Pain-An Overview of the Literature from 2005 to 2015. J Cardiothorac Vasc Anesth. 2016; 30(3):762-72.
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016; 41(5):621-7.
- Tulgar S, Senturk O. Ultrasound guided erector spinae plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty. J Clin Anesth. 2017; 44:68.
- Krishna SN, Chauhan S, Bhoi D, Kaushal B, Hasija S, Sangdup T, Bisoi AK. Bilateral Erector Spinae Plane Block for Acute Post-Surgical Pain in Adult Cardiac Surgical Patients: A Randomized Controlled Trial. J Cardiothorac Vasc Anesth. 2019; 33(2):368-75.
- Macaire P, Ho N, Nguyen T, Nguyen B, Vu V, Quach C, Roques V, Capdevila X. Ultrasound-Guided Continuous Thoracic Erector Spinae Plane Block Within an Enhanced Recovery Program Is Associated with Decreased Opioid Consumption and Improved Patient Postoperative Rehabilitation After Open Cardiac Surgery-A Patient-Matched, Controlled Before-and-After Study. J Cardiothorac Vasc Anesth. 2018; S1053-0770(18):31039-5.
- Tsui BCH, Fonseca A, Munshey F, Mcfadyen G, Caruso TJ. The erector spinae plane (ESP) block: A pooled review of 242 cases. J Clin Anesth. 2018; 53:29-34.
- Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017; 118(3):474-475.
- Romero A, Garcia JEL, Joshi GP. The state of the art in preventing post thoracotomy pain. Semin Thorac Cardiovasc Surg 2013, 25(2):116-24.
- Leyva FM, Mendiola WE, Bonilla AJ, Cubillos J, Moreno DA, Chin KJ. Continuous erector spinae plane (ESP) block for postoperative analgesia after minimally invasive mitral valve surgery. J Cardiothorac Vasc Anesth 2018, ;32(5):2271-74.
- Forero M, Rajarathinam M, Adhikary S, Chin KJ. Continuous ESP block for rescue analgesia in thoracotomy after epidural failure: A case report. AA Case Rep 2017; 8(10):254-6.
- Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: a retrospective cohort study. Anaesthesia. 2019; doi: 10.1111/anae.14579. [Epub ahead of print].