Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/131
Review Article OPEN ACCESS
Nursing Stroke Patients
Gill Cluckie, PhD, RCN1 and Anthony G Rudd, CBE, FRCP2*
1Consultant Stroke Nurse, St Georges Hospital, London, UK
2Emeritus Professor Stroke Medicine, School of Population Health & Environmental Sciences, Kings College London, United Kingdom
Anthony G Rudd, CBE FRCP, Emeritus Professor Stroke Medicine, School of Population Health & Environmental Sciences, Kings College London, Addison House, London SE1 1UL, United Kingdom, Tel: +44-7751-310953
Editor: Henry Liu, MD, MS, FASA, Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine, Penn State Milton S.Hershey Medical Center, 500 University Drive, PO Box 850, Mail code H187, Hershey, PA 17033-0850, USA; Tel: 717-531-5167; Fax 717-531-7790; E-mail: henryliupa@gmail.com
Received: October 08, 2020 | Accepted: December 03, 2020 | Published: December 05, 2020
Citation: Rudd AG, Cluckie G. Nursing Stroke Patients. Transl Perioper & Pain Med 2021; 8(1):298-304
Abstract
Stroke worldwide is the second most common cause of death and one of the most important causes of severe adult disability. While there have been major advances in the development of acute treatments such as endovascular thrombectomy, many patients will not make a rapid recovery and will need rehabilitation and often prolonged care. Nurses are vital members of the acute admitting team and have a central role on the stroke unit and in the delivery of longer term rehabilitation and support. In many countries these roles are not fully realized. This article highlights some of the evidence supporting the need for stroke specialist nurses and identifies the key skills required.
Introduction
It is not many years ago that stroke was regarded as an untreatable disease of older people, not really worth of attention or research and not an area that any self-respecting nurse would choose to work in. Clearly that has changed with evidence now showing that high quality coordinated care can transform a person with stroke from a life living with severe long-term disability to independence or from an unbearable life with disability to one which is bearable. While stroke physicians, neurologists, and therapists all have important roles to play in the treatment of stroke, it is the nursing staff who play the pivotal role, whether in the emergency department supporting the initial assessment and triage of stroke patients, supporting the delivery of intravenous thrombolytics or thrombectomy or on the stroke unit managing the acute stroke, preventing complications and delivering much of the rehabilitation. They then have important roles after discharge supporting care in the community, both in terms of rehabilitation, provision of psychological support and ensuring that secondary prevention is optimized.
There is increasing evidence supporting the vital role of the nurse [1]. Using data from the national audit of stroke in the United Kingdom it has been shown that if nurse staffing levels fall below about 3 nurses per 10 beds on the stroke unit on duty at any one time the chances of dying increase significantly [2].
Nurse staffing levels: Adjusted Hazard Ratio of 30-day Mortality of Patients Admitted on Weekends, by Ratio of Registered Nurses Per Ten Beds on the Weekend. (Figure 1).
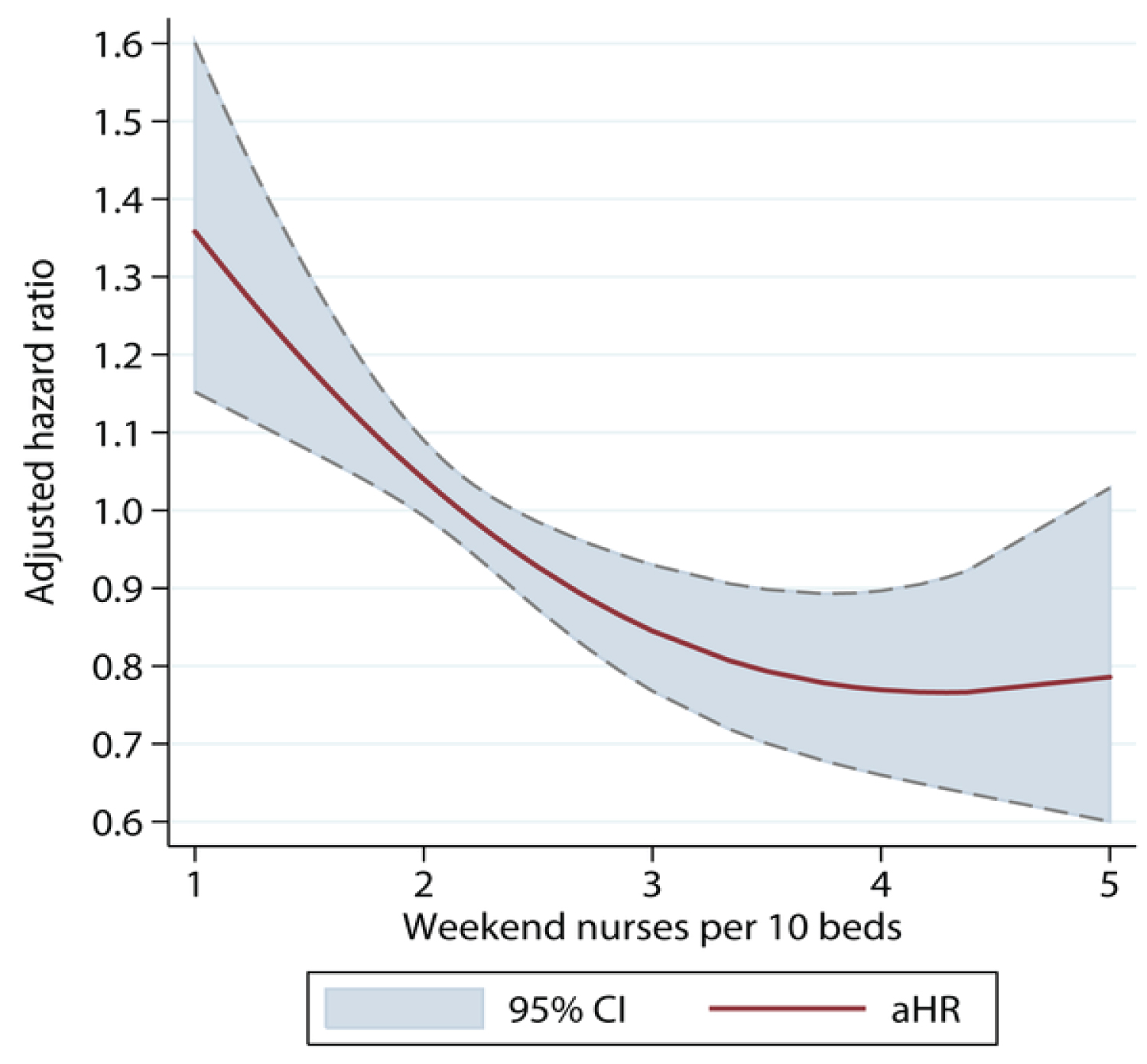
Figure 1: Nurse staffing levels: Adjusted hazard ratio of 30-day mortality of patients admitted on weekends, by ratio of registered nurses per ten beds on the weekend.
Using data from the same source, the association between different processes of care and mortality highlights the importance of some of the basic aspects of stroke nursing care in determining a good outcome [3]. Impact of care processes on odds of death at 30 days after stroke (Figure 2).
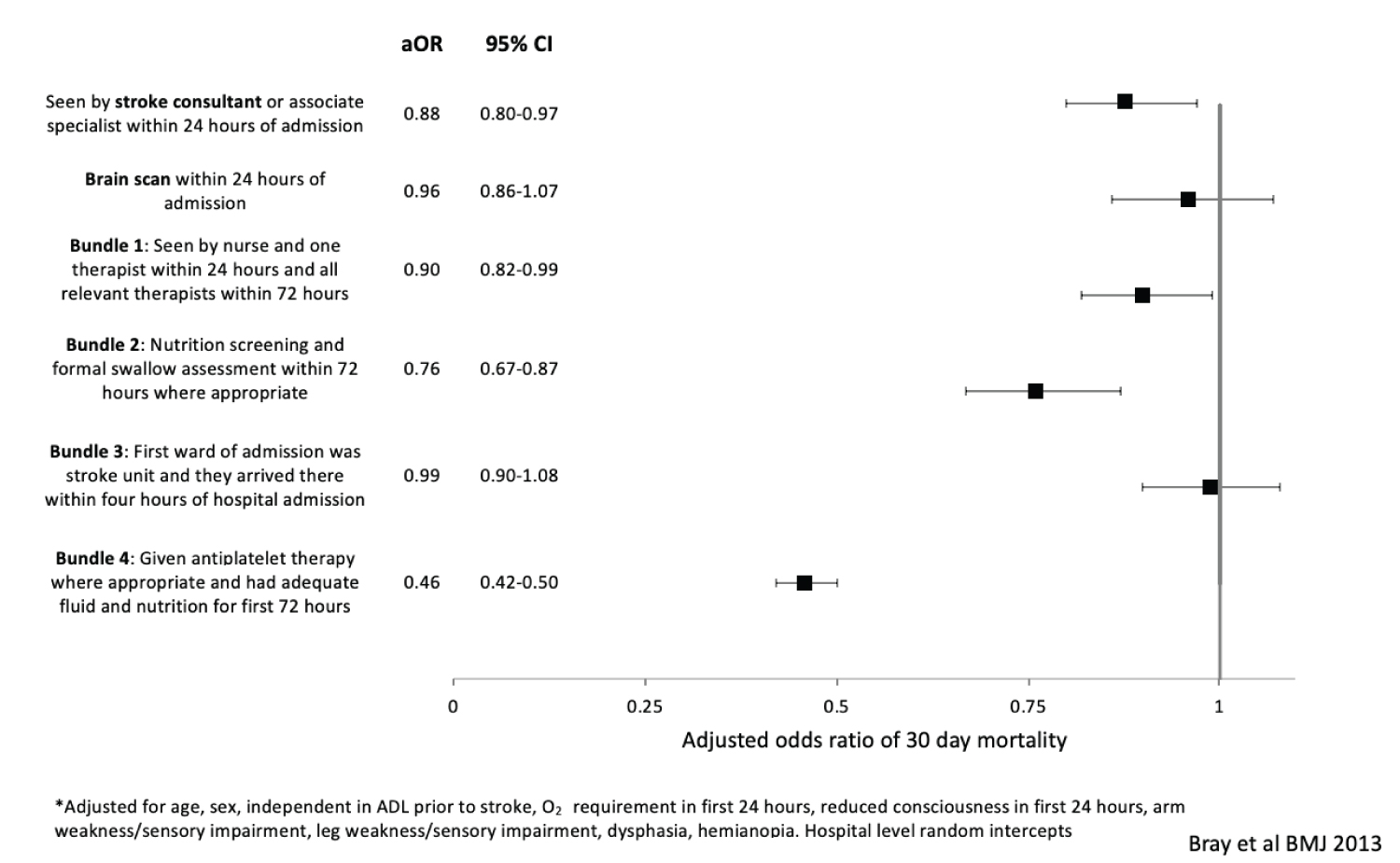
Figure 2: Impact of care processes on odds of death at 30 days after stroke*.
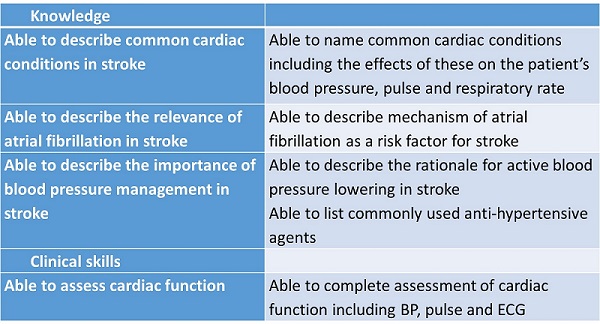
Stroke Nurse Competency Framework
As part of the process of improving stroke care in London, a group of senior stroke nurses developed a document outlining the key competencies that all nurses should achieve [4]. Some are core nursing skills that all nurses should have, others are specific to stroke. In this chapter we will cover some of the main stroke specific issues. Although developed for nurses in London it has relevance for all stroke services internationally. It will not attempt to comprehensively cover all aspects of care. Ultimately working in a good stroke service that is providing high quality specialist care from admission through to the longer term in the community, is the best way to understand the huge potential for specialist stroke nursing. Domains for stroke nursing skills included in the London Stroke Nurse Competency Framework (Table 1).
Table 1: Domains for stroke nursing skills included in the London stroke nurse competency framework.
|
Competency 1: Acute neurological care Competency 2: Thrombolysis and thrombectomy care Competency 3: Respiratory care Competency 4: Cardiovascular care Competency 5: Management of sepsis and infection control Competency 6: Diabetes care Competency 7: Nutrition and hydration Competency 8: Bladder and bowel continence Competency 9: Rehabilitation after stroke Competency 10: Fatigue after stroke Competency 11: Positioning and pressure area care Competency 12: Pain control Competency 13: Vision and perception Competency 14: Communication Competency 15: Psychological care Competency 16: Sex after stroke Competency 17: Self-administration of medicine Competency 18: Transfer of care Competency 19: Long term care Competency 20: End of life care |
Neurological assessment and care
A core role for stroke nurses is the monitoring and management of neurological status. This is often very frequent in hyper-acute stroke care where observations may be needed every 15 minutes. The aim of neurological observations is to identify any early deterioration and institute management to prevent long term consequences.
◼ Causes of deterioration
⚬ New neurological damage e.g. recurrent stroke, hemorrhagic transformation
⚬ Intercurrent illness e.g. infection
⚬ Epilepsy
⚬ Drug side effect
◼ What to measure
⚬ Conscious level e.g. Glasgow coma score (GCS)
⚬ National Institute of Health Stroke Score (NIHSS)
⚬ Pupil responses
⚬ Motor function
⚬ Vital signs
Thrombolysis and Thrombectomy
In the UK as in many other countries, the stroke nurse will often be the first person to assess the patient in the emergency department and it is important that they are aware of the acute treatments that are available for revascularization and know when to urgently initiate the thrombolysis and thrombectomy pathway. They need to know the key inclusion and exclusion criteria and be able to do a basic structured neurological assessment, including the Glasgow Coma Score (or similar screening tool for level of consciousness) and National Institute of Health Stroke Score (NIHSS). It is important that they know the evidence behind treatment including the risks, such as causing hemorrhage, so that they can explain to the patient and family what is proposed and why [5]. So, they also need good communication skills and have an understanding of mental capacity assessment so that they can judge how much decision making needs to be delegated to the family and clinical team.
Thrombolysis
The nurse should understand the action and contraindications of thrombolysis treatment.
• Recombinant tissue plasminogen activator (rt-PA) activates the release of plasminogen which converts to plasmin
• Plasmin is the enzyme that degrades fibrin
• Fibrin is the protein which is the main constituent of blood clots
Dose
The treatment is delivered in a dose based on the patient's weight and nurses should be able to calculate the correct dose of thrombolytic agent and know how to mix and administer the drug. They should alsobe able to institute the protocol for the management of blood pressure following thrombolysis including the use of intravenous agents such as labetalol or nicardipine. A standardised protocol will assist nurses in their management of blood pressure agents. The nurse will need to continue to monitor the patient's cardiovascular and neurological status and manage complications such as anaphylaxis and neurological deterioration.
Common post-thrombolysis complications
• Angioedema - 1.3%. It is more common with patients on ACE inhibitors
• Intracerebral hemorrhage - 1.7% (1 in 77 patients). 0.28% fatal
• Major Hemorrhage outside the brain- 0.4%
• Minor bleeding is common (e.g. IV site, gums)
Monitoring following thrombolysis
It is recommended that frequent neurological observations are undertaken following thrombolysis:
• Neurological observations: Observing for signs of neurological changes including nausea, vomiting, headache, seizure and informing doctors Every 15 minutes for the first 2 hours
Every 30 minutes for the following 2 hours
Every 60 minutes until 24 hours
• Blood pressure: Maintaining systolic BP below 180 mmHg and diastolic below 110 mmHg using the protocol agreed for the hospital. Often in the UK a bolus of IV labetalol 10-20 mg is used, repeated if necessary after 10 minutes. Alternatives include nicardipine or glyceryl trinitrate (GTN) [6].
Thrombectomy [7]
For patients undergoing thrombectomy the skills are similar but there also needs to be a thorough understanding of the process that the patient will be going through and for some nurses there will be a need to provide support for the interventional neuroradiologist in the operating theatre. Post-thrombectomy care will include monitoring of the groin puncture site and observation of the associated leg for signs of vascular compromise e.g. absent pulses, discoloration. Nurses should be able to monitor the groin puncture site for signs of bleeding or hematoma development. Post-thrombectomy observations will otherwise be similar to thrombolysis care and careful blood pressure management is also important.
Cardiovascular and respiratory care
Many of the complications that arise after stroke are related to cardio-respiratory problems. The nurse is key to recognizing these and initiating management. A frequent scenario is the patients deteriorating during the night when medical staff may not be present. Failure to immediately recognize this, the patient will have to wait till the doctor arrives in the morning. This will often mean that the best chances of effective treatment will be missed and patient care will be significantly be compromised. Stroke nurses need to be familiar with the basics of cardiorespiratory physiology and pathology and be able to do a basic assessment of function.
Ability to recognise dysrhythmias on a cardiac monitor and ECG, particularly life threatening arrhythmias such as ventricular tachycardia and important rhythms such as atrial fibrillation (AF) are important.
AF is very common and is a major predisposing factor for stroke [8]. Over 4% of people over 65 years and 10% of people over 75 years have AF. About 20% of strokes in the UK are secondary to AF and the strokes are often severe. Anticoagulants (warfarin or direct oral anticoagulants) reduce the risk of stroke by about 66%.
Stroke specialist nurses should be able to monitor the patient for the following parameters:
• Cardiac Rhythm - monitor for arrhythmias e.g. AF
• Blood Pressure - maintain adequate cerebral perfusion pressure (CPP)
• Respiratory rate/Oxygen saturations (detect and treat hypoxia) - maintain oxygen saturations > 95%
Knowing the hospital protocols for the management of hypotension and hypertension after both ischemic stroke and hemorrhagic stroke is essential. Blood pressure monitoring is critical even though there will be times when the best treatment for raised blood pressure is just to watch and not treat. Aside from those receiving thrombolysis or post-thrombectomy, acute anti-hypertensive treatment in people with acute ischemic stroke is recommended only if there is a hypertensive emergency such as encephalopathy, nephropathy or cardiac failure. Anti-hypertensive treatment in patients with intracerebral hemorrhage and a blood pressure above 150 mmHg should be aiming to get blood pressure below 140 mmHg for at least the first 7 days after the stroke [9].
Stroke can affect the function of the respiratory system directly (e.g. neural control of breathing) or indirectly (e.g. immobility reducing lung volumes) [10]. For example stroke can cause:
• Respiratory muscle dysfunction - stroke can cause chest wall muscle weakness and decreased diaphragmatic excursion. This can lead to decreased lung volumes (forced vital capacity, forced expiratory volume and peak expiratory flow rate)
• Cheyne-Stokes respiration. This is a form of periodic breathing characterized by periods of central apnea or hypopnea alternating with periods of hyperpnea. This is most often seen after brainstem and large bilateral cerebral strokes associated with a worse prognosis for stroke
Nurses' understanding the difference in cause and management of type 1 and type 2 respiratory failures and how stroke may result in problems is vital. Particularly important is recognizing changes in respiratory performance that might indicate the development of common respiratory complications such as pulmonary embolism or pneumonia. Regular monitoring of the patient's respiratory status including rate, pattern, depth, oxygen saturations and presence of any additional signs such as wheeze or crackles will be an early indicator of respiratory compromise. Ensuring good positioning particularly in upright positions can increases lung volumes, reduce the work of breathing, reduce central venous pressure and reduce the work of the heart (reduced preload).
The role of the nurse in respiratory care includes:
• Managing the airway including use of airway adjuncts or suction as indicated
• Continuous oxygen saturation monitoring in hyper-acute phase
• Early identification of respiratory compromise
• Provision of supplementary oxygen as indicated
• Treatment of aspiration pneumonia including antibiotics
• Optimal and regular repositioning
• Support and reassurance to patients experiencing respiratory symptoms
Sepsis and infection
One of the key roles of the stroke nurse is to identify the deteriorating patient, which will often be as a result of the development of sepsis. Both chest infection and urinary tract infections are common [11]. Chest infection can largely be prevented by early identification of dysphagia and the nurse has a key role in undertaking swallow screening looking for dysphagia. Impact of stroke on swallowing (Table 2).
Table 2: Impact of stroke on swallowing.
| Pre Oral | ➢ Reduced awareness, reduced salivation | |
| Oral | • Voluntary - chewing and preparation (saliva) | ➢ Facial, mouth and tongue weakness |
| Pharyngeal | • Involuntary - transporting bolus from the back of the mouth through the pharynx • Airway is protected | ➢ Pharyngeal weakness, incoordination of swallow, incomplete epiglottis closure |
| Oesophageal | • Involuntary - transportation of the bolus to the stomach | ➢ Reduced peristalsis |
Evidence from the UK national stroke audit has shown that the longer it takes to perform the swallow screen the greater the chance of developing pneumonia [12]. Time to dysphagia screen and risk of stroke-associated pneumonia (Figure 3).
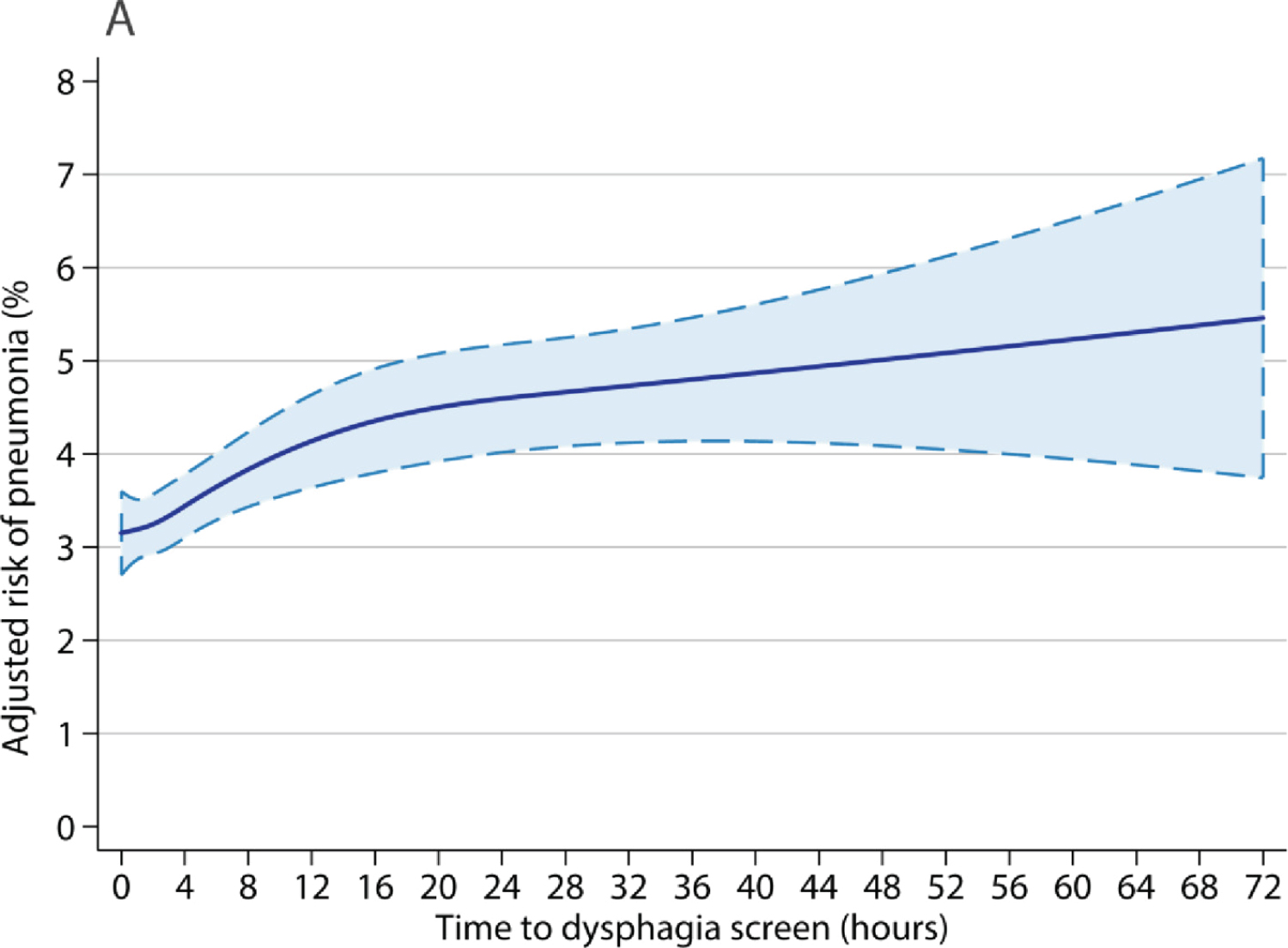
Figure 3: Time to dysphagia screen and risk of stroke-associated pneumonia.
Knowing how to modify food and liquid consistency and to position the patient appropriately for eating to enable safe swallowing or where necessary managing enteral tube feeding are core skills. However, the patient will still need careful monitoring and the nurse will need to know the signs of sepsis and how to initiate management.
Because dysphagia is so common after stroke and because the risks of aspiration are so high all patients with suspected stroke should have their swallow assessed as a matter of urgency on admission to hospital and this should usually be done using a bedside swallow assessment by the nurse or admitting doctor. It should only be done when the patient is awake, alert and able to be sat upright, should be done with clean water and no food, drink or medication prior to a swallow screen being performed. It should not be done in an unconscious patient or one who is too drowsy to sit upright or stay awake for 20 minutes. If the patient is assessed on screening as being at risk of aspiration then the patient should be seen promptly by a speech and language therapist for more detailed assessment, that may require instrumental assessment e.g. videofluroscopy or endoscopic evaluation of swallowing. An example of a bedside swallow screen (Figure 4).
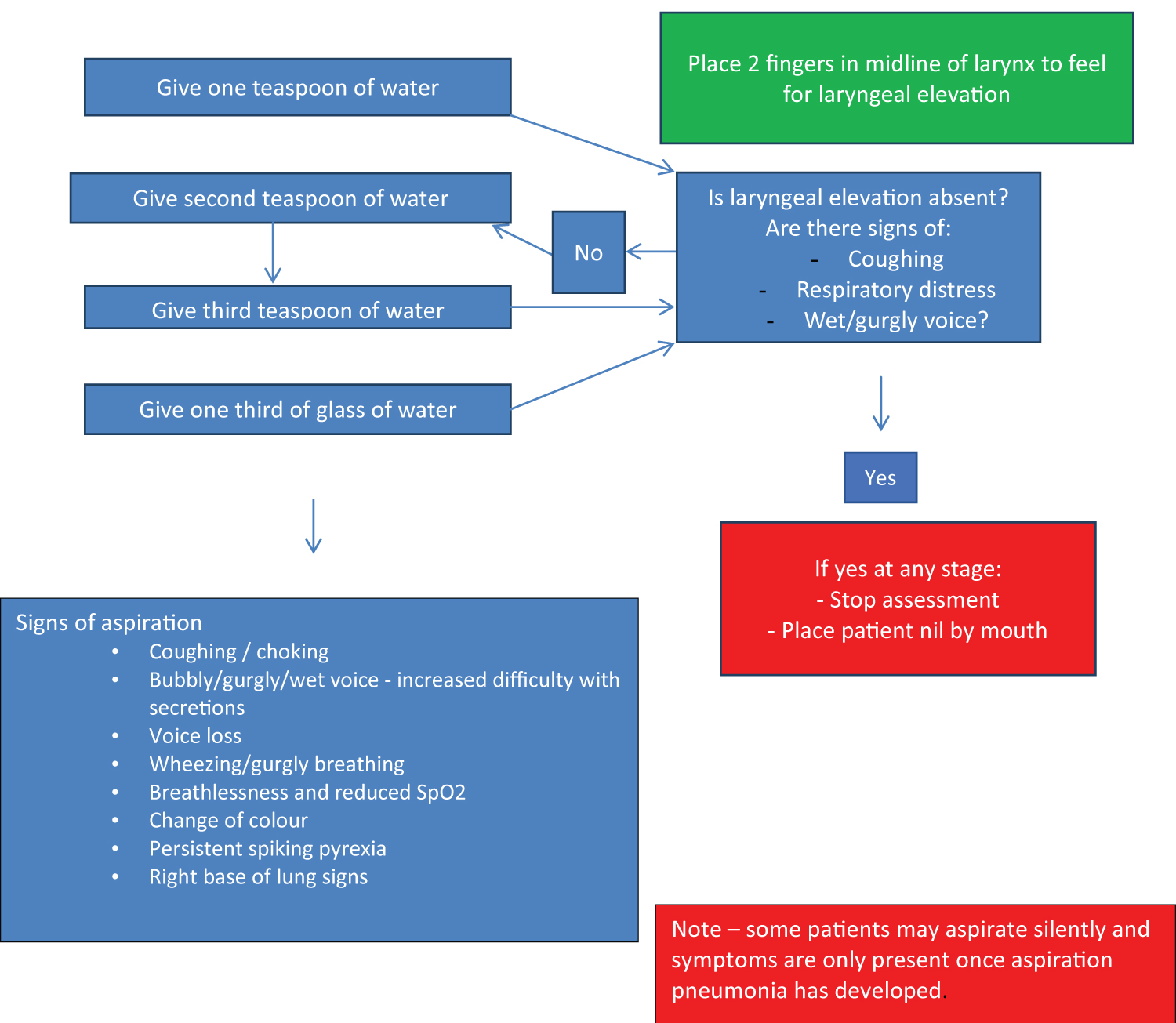
Figure 4: An example of a bedside swallow screen.
Nutrition and stroke
Malnutrition is defined as a body mass index (BMI) < 18.5 kg/m2 or unintentional weight loss of 5-10% within the last three to six months. It is well recognised that about 25% of patients become more malnourished in the first weeks after a stroke and malnutrition is an independent predictor of poor outcomes, mortality and length of stay [13]. Factors that may influence nutrition following stroke (Table 3).
Table 3: Factors that may influence nutrition following stroke.
|
Physical |
Psychological |
Organisational |
|
Dysphagia Drowsiness Hemiparesis Visual impairment Cognitive impairment Pain GI symptoms Co-morbidities e.g. diabetes Poor dentition Sore or dry mouth Oral thrush Changes in taste and smell Polypharmacy |
Depression Anxiety Bereavement Mental illness Apathy Poor motivation Loneliness Self-esteem Independence Substance abuse |
Lack of feeding assistance Adapted cutlery Inappropriate menu choices Unfamiliar foods Cold food Timings of meals Interruptions to mealtimes Rushed mealtimes Ward environment Ward culture Staff knowledge |
There is some evidence that following stroke and brain injury there is an increase in nutritional requirements [14]. This is exacerbated when there is fever or inflammation, an open wound or high activity levels. All patients admitted with stroke should have a nutritional screen completed to identify their risk of malnutrition. One such example is the MUST tool [15]. Example of a nutritional screening tool - MUST (Figure 5).
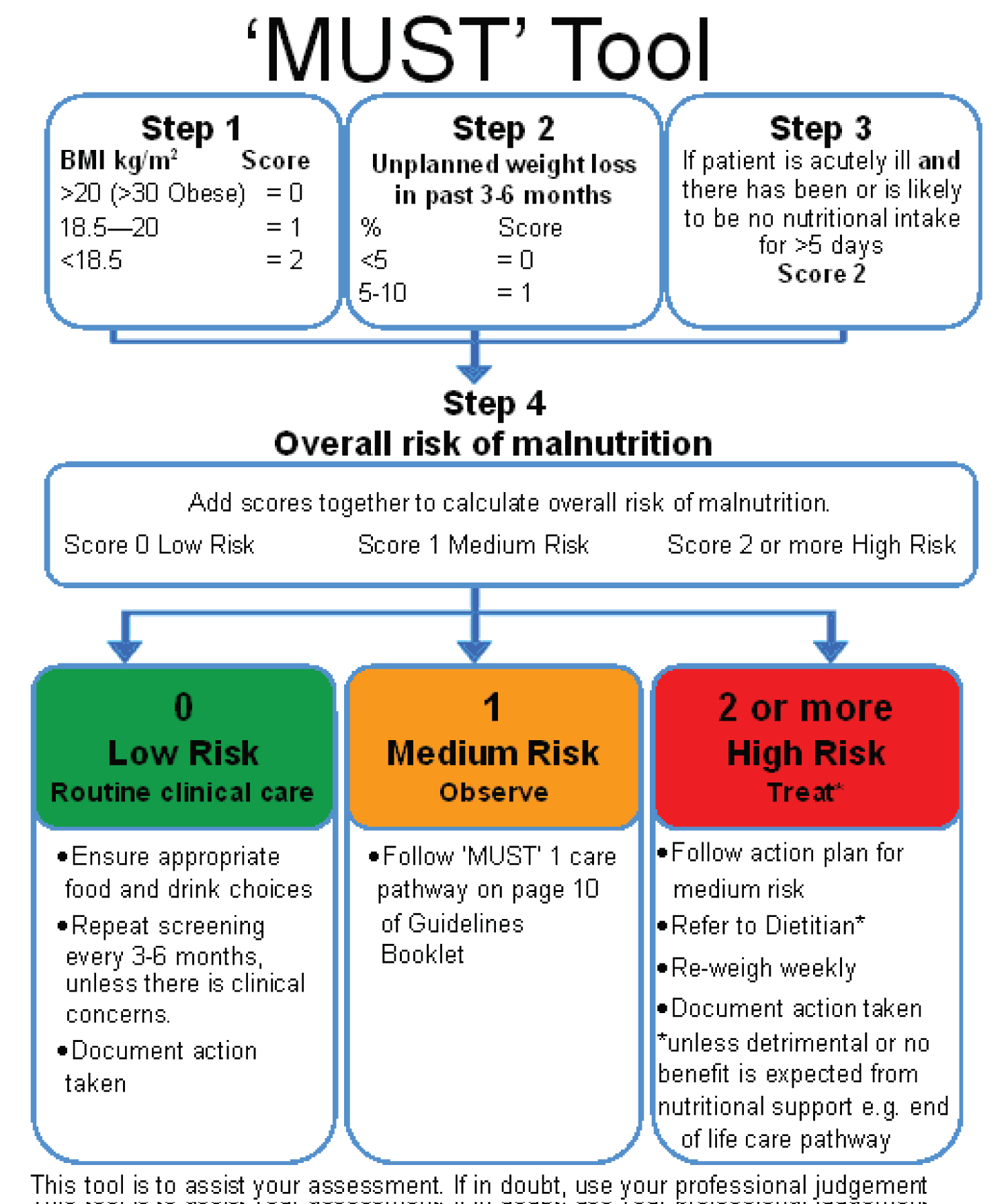
Figure 5: Example of a nutritional screening tool - MUST.
Nurses should be competent to insert nasogastric tubes and be able to care for nasogastric and gastrostomy tubes when they are in place. They need good communication skills to be able to explain to patients and their families the importance of the nutritional plan, including why it might be necessary to stop oral feeding or restrict the sorts of food and drink a patient is allowed.
Maintenance of hydration is vital after stroke. Nurses should be competent to monitor fluid intake, assess patients for signs and symptoms of dehydration and be competent to manage intravenous infusions.
Bladder and bowel
Both bladder and bowel dysfunction are common after stroke [15]. Nurses should understand different types of urinary incontinence and urinary retention, their possible causes and how each is best managed. Common causes for urinary incontinence in stroke (Table 4).
Table 4: Common causes for urinary incontinence in stroke.
|
|
Causes |
Symptoms |
Post-void bladder volume |
|
Urge |
Detrusor instability |
Urge, enuresis, large volumes |
Low |
|
Stress |
Sphincter insufficiency |
Triggers e.g. coughing Small volumes, high frequency |
Low |
|
Overflow |
Outlet obstruction |
Small volumes, frequency, abdominal discomfort |
High |
|
Functional |
Environment, cognition, physical impairments |
Varied volumes |
Low |
Urinary incontinence
A continence assessment should be undertaken on all patients with urinary incontinence to determine the type and identify suitable treatment strategies. Bladder scanning should be a routine component of continence management.
A continence assessment should include the following:
• Patient history
• Urinalysis
• Urine specimen to check for UTI
• Clinical examination e.g. palpable bladder
• Rectal examination e.g. to rule out constipation, enlarged prostate
• Post-void bladder scan
• Continence chart - frequency, volume
• Medication review
Urinary catheters should be avoided unless there is urinary retention that cannot be rapidly resolved and they should not be used as a tool for continence management. Continence promotion should be commenced early to encourage the patient to regain control of their bladder function. Whilst incontinence is present careful monitoring and management of the skin is vital to prevent moisture associated damage or pressure area breakdown.
Fecal incontinence and constipation
often cause great distress to patients but can usually be effectively managed with good nursing and medical care [16]. Nurses need to understand the underlying causes and be able to develop and implement a bowel management plan including the appropriate use of laxatives. A bowel assessment should include the following:
• Stool chart - frequency and consistency
• Use of visual tool for stool e.g. Bristol stool chart
• Clinical examination
• Rectal examination
• Medication review
The role of the nurse in continence management and promotion is:
• Assessment and identification of causes of incontinence
• Ensuring good skin integrity and preventing skin breakdown
• Treating reversible causes e.g. UTI or constipation
• Implementing a continence management plan to promote continence
• Avoiding urinary catheters as a tool for managing continence
• Support and advice for patients and relatives
Positioning and Pressure Area Care
The nursing staff within stroke services should complete a risk assessment of the patient's capabilities. This assessment should follow a standardised tool which assesses each individual patient and consider the following:
• The individual patients ability to be independent
• The individual patients physical, communication and cognitive abilities
• The individual patients pre-admission mobility including any aids used
• All potential manual handling required including moving in bed, transferring from bed to chair, sitting, standing and walking as appropriate
• Equipment and staff required to achieve a safe outcome
The manual handling plan should be available for all staff and should clearly document what assistance the patient requires. Particularly for the hemiplegic and frail patients the nurse has a key role in ensuring good positioning of the patient both in bed and when they are sitting out in a chair. Failure to do so can result in spasticity, contractures, pressure sores, musculoskeletal pain, shoulder pain and subluxation and aspiration pneumonia. Skilled moving and handling of the patient is important for both the patient and to maintain a healthy nurse who does not end up with back pain that prevents him or her working.
Key nursing activities related to positioning and manual handling:
• Seating - use of specialist chairs/external supports/pillows
• Bed positioning
• Splinting/orthosis
• Positioning and stretches
• Individual sessions e.g. active exercises
• Within functional activities e.g. use of shower, toilet, transferring, walking
• Education and handling advice
• Environmental changes
• Medication
Pressure sores that develop in hospital should be seen as a failure of medical and nursing care. They can nearly always be avoided by regular relief of pressure through regular turning and the use of pressure relieving equipment such as mattresses and cushions. Poorly managed continence can also contribute to macerated skin and subsequent skin breakdown and pressure sores. On admission and at frequent intervals patients should have their risk of pressure area breakdown assessed by a standardised assessment tool such as the Waterlow score [17]. There should be daily checks of pressure areas such as sacrum and heels for any signs of skin discoloration, blistering or ulceration. Pressure sore risk reduction should include regular repositioning, adequate mattress e.g. air mattress, adequate nutrition and hydration and the reduction of shearing forces during repositioning.
The hemiplegic shoulder is specifically at high risk for damage and careful positioning and handling can prevent deterioration [18]. Subluxation due to muscle weakness makes the hemiplegic shoulder particularly high risk of damage due to poor handling. Patients should never be handled under their arm and families should be educated in safe handling techniques. Support under the hemiplegic arm e.g. with cuffs or pillows can reduce the drag on the shoulder joint. Prevention of shoulder damage is particularly important as once it has occurred it can take many months to improve and severely impair recovery of limb function.
Nurses roles in positioning and pressure care include:
• Prevention of spasticity
• Optimal manual handling plan in place
• Prevention of pressure area or skin breakdown
• Daily observation of high risk skin areas
• Education of patient and families
• Careful positioning and support for hemiplegic shoulder
Management of the agitated or confused patient
Delirium is common after stroke [19], either as a result of the structural brain damage or because of co-morbidities, such as infection. It is more likely to occur in people with pre-existing dementia. Wherever possible medications should be avoided as these can exacerbate the problem and hinder rehabilitation. Skilled nursing through frequent reorientation, ensuring the patient is managed in a calm, quiet, well-lit environment and avoiding restraints will often be sufficient to calm the patient. Rapid diagnosis of delirium and investigation and treatment of the cause will minimise the severity and duration of a delirium.
Rehabilitation
Nurses are key members of the rehabilitation team. Therapists may see the patient for an hour or two a day. The nurses are responsible for maintaining a rehabilitation ethos for the patient for the whole 24 hours. They should be involved in the multidisciplinary meetings that should be held to plan the care of all the patients and play an active role in setting goals. They should be aiming to support the patient to be as independent as possible even if that means that caring for the patient takes longer than if the nurse was to do everything for them. Very often it will be the nurse who knows the patient better than any other member of the team so the nurse may need to act as the spokesperson for the patient.
Vision and Perception
Paralysis is usually very obvious. But some less evident stroke deficits may be equally or more disabling. Nurses should be able to recognise visual field defects such as hemianopia and visual neglect and understand how these can affect function and how they should be taken into account in supporting a patient's treatment and recovery. Similarly, sensory loss or sensory perceptual problems need to be identified and taken into account in managing the patient.
Nurses should be aware of the nature of hemianopia and the impact this has on daily activities such as walking and eating and drinking. They should encourage techniques such as visual scanning and regularly orientate the patient to their difficulties. Nurses should be aware of neglect and its potential impact on daily activities such as washing and dressing.
Communication
Some of the most distressing problems that stroke patients can suffer from are communication difficulties -dysphasia, dysarthria and orofacial dyspraxia [15]. It is important that nurses understand the implications of communication difficulties and learn how to communicate best with such patients. Most important is to understand that the dysphasic patient is not globally cognitively impaired and therefore not to assume that the patient is incapable of rational thought. It is likely to be necessary for the nurse to work closely with the speech therapist and the family to maximize the patient's recovery.
Nurses should work with the speech therapists to establish a consistent communication method for patients to ensure they are able to communicate their needs. Where this is not possible nursing staff will need to anticipate care needs and to observe for non-verbal signs e.g. facial expression, gesture. Closed questions with a yes/no response may be more suitable and some patients will require pictorial communication support.
Psychological Care
Unfortunately, few stroke services have adequate access to psychologists to provide sufficient support and treatment to patients who often have multiple cognitive and emotional problems resulting from the stroke and sometimes pre-existing conditions [20]. Nurses therefore by default have to fill the gap. They need to understand the range of psychological and emotional problems that can result from stroke and the impact that stroke can have on the family and friends. And they need to then be able to provide basic psychological support and know when it is necessary to refer on to scarce psychological services for additional help.
Challenging behavior can also develop as a result of stroke and lead to difficult situations on the ward with aggressive or offensive behavior to staff, other patients and family. Skilled nursing is often needed to defuse and manage these sorts of situations.
Long Term Care
The transition from hospital to home can be traumatic for patients and their carers, particularly if significant disability persists. While continued physiotherapy, occupational therapy, speech therapy and psychology if available, will be invaluable for some patients, nurses have a major role to play both in coordinating care and ensuring that a holistic approach is taken as well as providing specialist nursing functions. A trial from China currently underway should provide interesting data on some of these aspects of care [21]. Nurses have a key role in supporting patients in the longer term including supporting self-management [22] and encouraging effective strategies for stroke prevention [23].
End of Life Care
Unfortunately, there will always be some patients whose strokes are so severe that recovery is not possible and the most important role for the clinical team is to ensure whatever life remains is spent as comfortably as possible. Fortunately, stroke is not usually painful but the last days and weeks of life can nevertheless be very distressing for the patient and their family. Nurses must play a central role in managing both the physical and psychological issues [24]. They need to have an understanding of how to manage anxiety, depression dyspnoea, constipation and sometimes pain. They need to work with the multidisciplinary team to ensure there is a comprehensive plan that is then delivered. They need to be equipped to deal with the grief of the family and friends and understand the ethical issues in the context of the cultural values of the country that they are working in [24].
Summary
Stroke nursing is a highly skilled and complex job requiring expertise in medicine, nursing, psychology and many other fields. It is not just about making beds, cleaning up soiled sheets and bodies and administering drugs. Nurses must not be seen as being subservient to the physicians. Rather they should be seen as equal partners providing a vital role in the management of the patient and their family. It is a specialty that needs the best, brightest, most hard working and humane nurses that there are.
References
- Theofanidis D, Gibbon B. Nursing interventions in stroke care delivery: An evidence-based clinical review. J VascNurs. 2016;34(4):144-151. doi:10.1016/j.jvn.2016.07.001
- Bray BD, Ayis S, Campbell J, Cloud GC, James M, Hoffman A, Tyrrell PJ, Wolfe CD, Rudd AG. Associations between stroke mortality and weekend working by stroke specialist physicians and registered nurses: prospective multicentre cohort study. PLoS Med. 2014 Aug 19;11(8):e1001705. doi: 10.1371/journal.pmed.1001705. PMID: 25137386; PMCID: PMC4138029.
- Bray BD, et al 2014 Associations between Stroke Mortality and Weekend Working by Stroke Specialist Physicians and Registered Nurses: Prospective Multicentre Cohort Study. PLoS Med 11(8): e1001705. doi:10.1371/journal.pmed.1001705
- London Stroke and Cardiac Networks. London Stroke Nurse Competency Workbook 2016; https://www.england.nhs.uk/london/wp-content/uploads/sites/8/2019/09/london-stroke-nurse-competency-workbook.pdf
- Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database of Systematic Reviews 2014, Issue 7. Art. No.: CD000213. DOI: 10.1002/14651858.CD000213.pub3.
- Appleton JP, Sprigg N, Bath PM. Blood pressure management in acute stroke. Stroke and Vascular Neurology 2016;1: e000020. doi:10.1136/svn- 2016-000020
- Lindekleiv H, Berge E, Bruins Slot KMH, Wardlaw JM. Percutaneous vascular interventions versus intravenous thrombolytic treatment for acute ischaemic stroke. Cochrane Database of Systematic Reviews 2018, Issue 10. Art. No.: CD009292. DOI: 10.1002/14651858.CD009292.pub2
- Reiffel JA. Atrial fibrillation and stroke: epidemiology. Am J Med. 2014 Apr;127(4):e15-6. doi: 10.1016/j.amjmed.2013.06.002. PMID: 24655742.
- Wajngarten M, Silva GS. Hypertension and Stroke: Update on Treatment. Eur Cardiol. 2019 Jul 11;14(2):111-115. doi: 10.15420/ecr.2019.11.1. PMID: 31360232; PMCID: PMC6659031.
- Howard RS, Rudd AG, Wolfe CD, Williams AJ. Pathophysiological and clinical aspects of breathing after stroke. Postgrad Med J. 2001 Nov;77(913):700-2. doi: 10.1136/pmj.77.913.700. PMID: 11677278; PMCID: PMC1742182.
- Berger B, Gumbinger C, Steiner T, Sykora M. Epidemiologic features, risk factors, and outcome of sepsis in stroke patients treated on a neurologic intensive care unit. J Crit Care. 2014 Apr;29(2):241-8. doi: 10.1016/j.jcrc.2013.11.001. Epub 2013 Nov 8. PMID: 24332993.
- Bray BD, Smith CJ, Cloud GC, Enderby P, James M, Paley L, Tyrrell PJ, Wolfe CD, Rudd AG; SSNAP Collaboration. The association between delays in screening for and assessing dysphagia after acute stroke, and the risk of stroke-associated pneumonia. J NeurolNeurosurg Psychiatry. 2017 Jan;88(1):25-30. doi: 10.1136/jnnp-2016-313356. Epub 2016 Jun 13. PMID: 27298147.
- Sabbouh T, Torbey MT. Malnutrition in Stroke Patients: Risk Factors, Assessment, and Management. Neurocrit Care. 2018 Dec;29(3):374-384. doi: 10.1007/s12028-017-0436-1. PMID: 28799021; PMCID: PMC5809242.
- Weekes E, Elia M. Resting energy expenditure and body composition following cerebro-vascular accident. Clin Nutr. 1992;11(1):18-22. doi:10.1016/0261-5614(92)90058-x
- Intercollegiate Stroke Working Party. National Clinical Guidelines for Stroke. 5th Edn 2016. https://www.rcplondon.ac.uk/guidelines-policy/stroke-guidelines Date accessed 21/11/2020
- Harari D, Coshall C, Rudd AG, Wolfe CD. New-onset fecal incontinence after stroke: prevalence, natural history, risk factors, and impact. Stroke. 2003 Jan;34(1):144-50. doi: 10.1161/01.str.0000044169.54676.f5. PMID: 12511766.
- Thompson D. An evaluation of the Waterlow pressure ulcer risk-assessment tool. Br J Nurs. 2005 Apr 28-May 11;14(8):455-9. doi: 10.12968/bjon.2005.14.8.17930. PMID: 15924028.
- Lindgren I, Jönsson A-C, Norrving B, Lindgren A. Shoulder Pain After StrokeA Prospective Population-Based Study. Stroke. 2007;38:343–348. https://doi.org/10.1161/01.STR.0000254598.16739.4e
- Shaw R, Drozdowska B, Taylor-Rowan M, et al. Delirium in an Acute Stroke Setting, Occurrence, and Risk Factors 2019;50:3265–3268. https://doi.org/10.1161/STROKEAHA.119.025993
- National Institute Health and Social Care Excellence (NICE). Psychological care after stroke Improving stroke services for people with cognitive and mood disorders https://www.nice.org.uk/media/default/sharedlearning/531_strokepsychologicalsupportfinal.pdf. Accessed 21/11/2020
- Lin S, Xiao LD, Chamberlain D. A nurse-led health coaching intervention for stroke survivors and their family caregivers in hospital to home transition care in Chongqing, China: a study protocol for a randomized controlled trial. Trials . 2020;21(1):240. doi:10.1186/s13063-020-4156-z
- Kidd L, Booth J, Lawrence M, Rowat A. Implementing Supported Self-Management in Community-Based Stroke Care: A Secondary Analysis of Nurses' Perspectives. J Clin Med . 2020;9(4):985. doi:10.3390/jcm9040985
- Parappilly BP, Field TS, Mortenson WB, Sakakibara BM, Eng JJ. Effectiveness of interventions involving nurses in secondary stroke prevention: A systematic review and meta-analysis. Eur J Cardiovasc Nurs . 2018;17(8):728-736. doi:10.1177/1474515118779732
- Lutz BJ, Green T. Nursing's Role in Addressing Palliative Care Needs of Stroke Patients. Stroke . 2016;47(12):e263-e265. doi:10.1161/STROKEAHA.116.013282