Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/140
Research Article | Volume 8 | Issue 3 Open Access
Impacts of COVID-19 Epidemic on Labor and Delivery: Data from Anesthesia Quality Control Registry of Hubei, China
Jing Wu1#, Jianjuan Ke2#, Jie Wang1#, Weimin Xiao1, Lingyun Ren3, Xin Yan1, Richard Month4, John Grothusen4, Xiangdong Chen1 and Shanglong Yao1*
1Department of Anesthesiology, Institute of Anesthesia and Critical Care Medicine, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China
2Department of Anesthesiology, Zhongnan Hospital, Wuhan University, Wuhan, Hubei, China
3Department of Anesthesiology, Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China
4Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, PA, USA
#Contributed equally as co-first authors
Shanglong Yao, MD, PhD, Professor and Director of the Institute of Anesthesia and Critical Care Medicine, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, 1277 Jiefang Avenue, Wuhan, Hubei 430022, China, E-mail: ysltian@163.comEditor: Yuan-Xiang Tao, Ph.D., M.D., Professor and Vice Chair, Director, Center for Pain Medicine Research, Department of Anesthesiology, Editor in Chief, The Translational Perioperative and Pain Medicine, Rutgers, The State University of New Jersey, New Jersey Medical School, 185 S. Orange Ave., MSB, E-661, Newark, NJ 07103, USA, Tel: 973-972-9812, E-mail: yt211@njms.rutgers.edu
Received: May 10, 2021 | Accepted: June 22, 2021 | Published: June 23, 2021
Citation: Wu J, Ke J, Wang J, Xiao W, Ren L, et al. Impacts of COVID-19 Epidemic on Labor and Delivery: Data from Anesthesia Quality Control Registry of Hubei, China. Transl Perioper & Pain Med 2021; 8(3):350-358
Abstract
Background: In this study, we investigated the impact of COVID-19 on obstetric care in general hospitals and women's hospitals in Hubei, China.
Methods: We sent a survey to investigate the changes of care for labor and delivery and to identify characteristics and outcomes of parturients contracted with COVID-19 between January and February of 2020 in Hubei.
Results: We received 138 valid responses from hospitals in Hubei with response rate of 61.9% (138/223) and identified 33,483 cases of labor and delivery from January 1 to February 25, 2020. The caesarean delivery rate was 49.9%; and average labor analgesia rate was 26.0%. Interestingly, more general hospitals did strict maternal triage, admission and isolation than women's hospitals, but more women's hospitals offered routine service for labor and delivery (96.3% vs. 73.9%) and labor analgesia (77.8% vs. 43.2%) than general hospitals. We found 83 confirmed COVID-19 patients for caesarean delivery (0.50%). The majority of the patients with COVID-19 had only mild to moderate symptoms. Most of them received epidural or spinal anesthesia without documented complications. No neonatal infection was detected.
Conclusions: During the pandemic, labor analgesia rates had not changed significantly in Hubei and labor analgesia can be safely performed for parturients, including those who have contracted COVID-19. Women's hospitals have shown higher capacity and quality of obstetric care than general hospitals, but general hospitals showed strength through the pandemic with control on maternal triage, admission and isolation.
Keywords
Coronavirus disease 2019 (COVID-19), Anesthesia, Cesarean delivery, Labor analgesia, Quality control
Introduction
SARS-CoV-2 induced disease (COVID-19) has rapidly spread across the globe with the ongoing pandemic creating an international public health emergency, since it was first detected in early December 2019 in Wuhan, the capital of Hubei province in China. Obstetrical patients, especially parturients in the third trimester, do not have an alternative treatment as non-obstetrical patients may have during the epidemic. And women during pregnancy and puerperium could potentially be a vulnerable population due to physiological changes in their immune and cardiopulmonary systems [1,2]. A few single-center studies reported clinical characteristics of pregnant women with confirmed COVID-19 who underwent caesarean deliveries and suggested spinal anesthesia was administrated safely with no evidence of vertical transmission in late pregnancy [3,4]. There is lack of large-sample, multicenter studies about the effects of COVID-19 on maternal and neonatal outcomes. China has high caesarean delivery rates partly due to a lack of adequate neuraxial labor analgesia services [5]. It is of interest to see how much impact the outbreak had on caesarean delivery and labor epidural analgesia rates. In China, patients with a suspected or confirmed diagnosis of COVID-19, including parturients for labor and delivery, are diverted to designated hospitals to receive proper management. It was unclear whether this practice would alter patient safety.
In this study, after monitoring for unusual data changes from the Quality Control and Service Cloud Platform of Anesthesia in Hubei for obstetric anesthesia during the early stage of the COVID-19 outbreak, we conducted a survey along with data reporting to investigate the overall status of care for labor and delivery during the COVID-19 outbreak. In designing this study, we aimed to: (1) Identify the impact of COVID-19 on anesthesia, mainly in obstetric care; and (2) Determine the characteristics, severity and outcomes of parturients with COVID-19 and the status of the neonates.
Methods
This study was approved by the institutional review board of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, and the requirement for written informed consent was waived, as this study was a retrospective observational study without patient interventions.
The Quality Control and Service Cloud Platform of Anesthesia in Hubei (https://www.medqc.com), which was established in 2009 as a data reporting platform of Anesthesia Quality Control Center (AQCC) of Hubei, collects hospital-level data every month from 323 hospitals in Hubei. For the purpose of anesthesia quality improvement during the COVID-19 outbreak, we designed a survey with voluntary cooperation from the platform of AQCC of Hubei to investigate the changes in obstetric anesthesia, and to identify infected parturients in Hubei during the time period of January 1 to February 25, 2020 (Appendix I, Survey). The survey was sent to the members of the AQCC of Hubei including Chairs or Vice-Chairs of the anesthesia departments and the departmental liaisons for quality control. To speed up the investigation, the survey was opened only for 5 days from 9:00 am on February 20, 2020, to 9:00 pm on February 25, 2020. Further medical record reporting and data analysis were performed for those patients with a suspected and/or confirmed COVID-19 diagnosis. Suspected cases are defined as presenting with a fever or any respiratory symptoms, especially in those with a history of travel to Wuhan or exposure to infected people within two weeks. Confirmed cases are defined as those who have symptoms and a positive viral test. The clinical types of COVID-19 are listed as Appendix II. We summarize our data collection process including inclusion and exclusion criteria in Figure 1. In addition, we also collected the monthly labor analgesia rates from AQCC from January 2019 to May 2020.
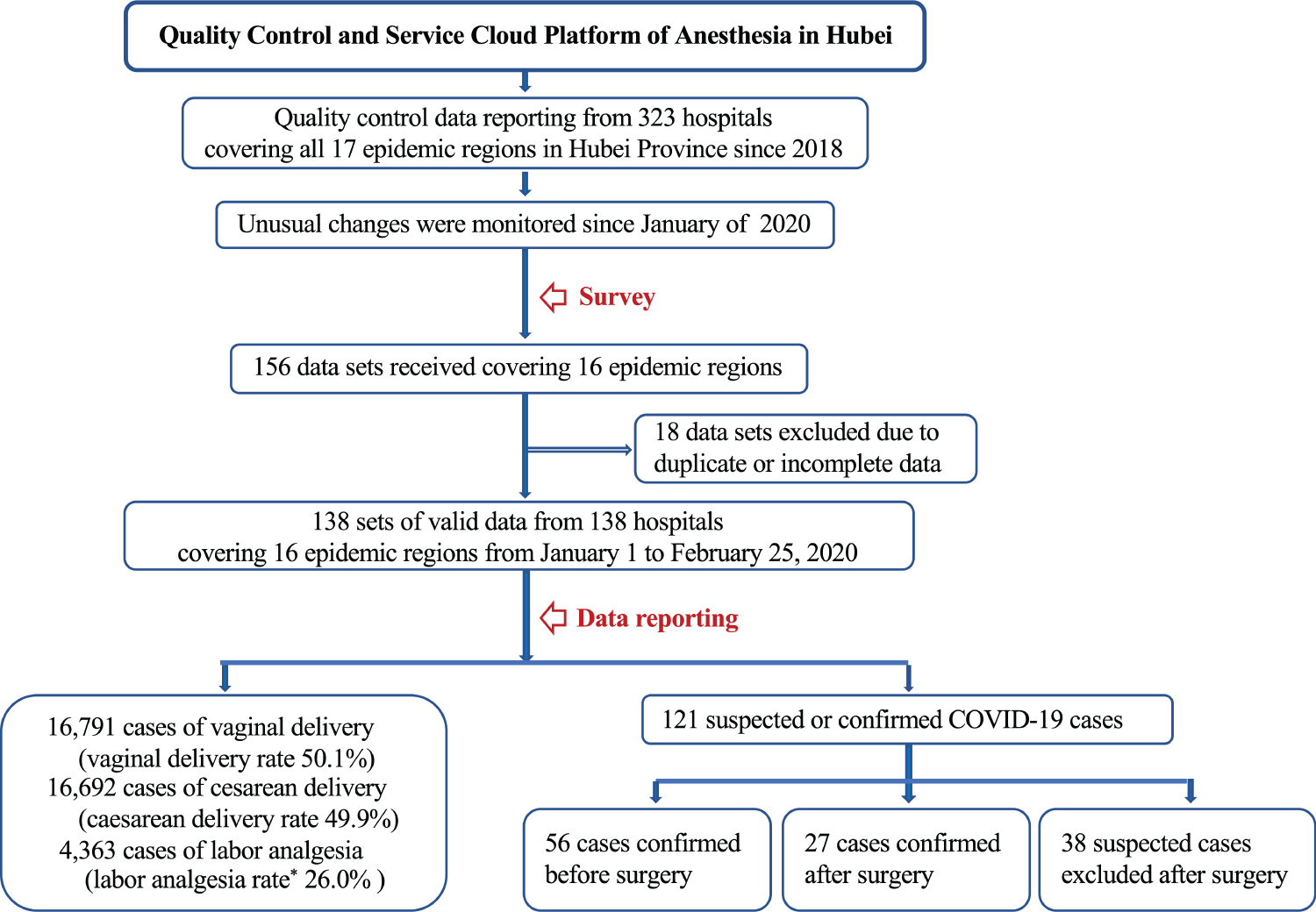
Figure 1:
Flowchart for the data collection.
Hubei province consists of 17 regions that are all defined as epidemic areas. Suspected cases are defined as presenting with a fever or any respiratory symptoms, especially in those with a history of travel to Wuhan or exposure to infected people within two weeks. Confirmed cases are defined as those who have symptoms and a positive viral test.
*labor analgesia rate = labor analgesia cases / vaginal delivery *100%
Primary outcome is the data for labor and delivery including cases of vaginal delivery, caesarean delivery and epidural analgesia for labor. Secondary outcomes are COVID-19 infection in patients with caesarean delivery including characteristics, clinical severity and maternal outcomes and those of the neonates.
Statistics
This study uses descriptive statistical analysis. Continuous variables were presented as mean ± standard deviation (SD) and compared by paired t-test. Categorical variables were expressed as number (%) and compared by χ2 test or Fisher's exact test. P values were 2-tailed with statistical significance set at 0.05. Statistical analysis was performed with SPSS (version 26.0, IBM. New York).
Results
We collected 138 sets of valid data from 138 hospitals from 16 (94.1%) of the 17 regions in Hubei Province, the epicenter of COVID-19 in China. From the reporting data of AQCC, 223 hospitals still offered the clinical service during January and February in 2020, so the response rate of the survey is 61.9% (138/223). Of these, 80.4% (111/138) of the data came from general hospitals while the rest 19.6% (27/138) from women's hospitals. And 81.2% (112/138) came from designated hospitals for COVID-19 patients. With regards to resource allocation, 90.5% hospitals allocated their anesthesiologists to clinical anesthesia and emergency intubation related to COVID-19, 14.6% assisted in the ICU, 8.8% in isolation wards and 8.0% in fever clinics. The data collection was completed primarily by departmental Chairs or Vice-Chairs (82.6%, 114/138) with the rest by departmental liaisons for quality control.
Care of labor and delivery changed during the pandemic
As shown in Table 1, 123 out of 138 hospitals (89.1%) set up fever clinics for screening to identify pregnant women with fever (temperature ≥ 37.3 °C) and 74 out of 138 hospitals performed routine lung computerized tomography (CT) scans for pregnant women to identify potential pneumonia (53.6%). The rate of routine viral nucleic acid RT-PCR from nasopharynx swab for pregnant women and infants was only 40.6% (56/138) and 29.7% (41/138), respectively. Interestingly, more general hospitals did stricter maternal triage than women's hospitals (routine CT, 60.4% vs. 25.9%, p = 0.0013; infant nucleic acid amplification test, 35.1% vs 7.4%, p = 0.0047), admission and isolation (admission through fever clinic, 79.3% vs. 59.3%, p = 0.0304; isolation or negative pressure wards, 57.7% vs. 29.6%, p = 0.0089; isolation or negative pressure operating room, 71.2% vs. 33.3%). However, more women's hospitals offered routine service for labor and delivery (96.3% vs. 73.9%, p = 0.0113) and labor analgesia (77.8% vs. 43.2%, p = 0.0013) than general hospitals. Only 5.1% (7/138) of the hospitals provided labor analgesia for pregnant women with suspected or confirmed COVID-19, including 44 confirmed cases and 42 suspected cases of labor analgesia, 43 confirmed cases and 36 suspected cases of planned vaginal delivery under labor analgesia converted to caesarean delivery.
Table 1: Triage, isolation and delivery services in 138 hospitals in Hubei (hospitals (%)).
|
|
Number (%) |
General hospital (n = 111) |
Women's hospital (n = 27) |
x2 |
p |
|
Maternal triage |
|
|
|
|
|
|
Fever clinics |
123 (89.9) |
99 (89.2) |
24 (88.9) |
0.1 |
0.7644 |
|
Routine CT |
74 (53.6) |
67 (60.4) |
7 (25.9) |
10.4 |
0.0013 |
|
Mother nucleic acid amplification test |
56 (40.6) |
49 (44.1) |
7 (25.9) |
3.0 |
0.0838 |
|
Infant nucleic acid amplification test |
41 (29.7) |
39 (35.1) |
2 (7.4) |
8.0 |
0.0047 |
|
Admission and isolation |
|
|
|
|
|
|
Admission through fever clinic |
104 (75.4) |
88 (79.3) |
16 (59.3) |
4.7 |
0.0304 |
|
Isolation or negative pressure wards |
72 (52.2) |
64 (57.7) |
8 (29.6) |
6.8 |
0.0089 |
|
Isolation or negative pressure delivery room |
38 (27.5) |
31 (27.9) |
7 (25.9) |
0.0 |
0.8346 |
|
Isolation or negative pressure operating room |
88 (63.8) |
79 (71.2) |
9 (33.3) |
13.5 |
0.0002 |
|
Labor and labor analgesia |
|
|
|
|
|
|
Routine service for labor and delivery |
108 (78.3) |
82 (73.9) |
26 (96.3) |
6.4 |
0.0113 |
|
Labor analgesia for routine labor and delivery |
69 (50.0) |
48 (43.2) |
21 (77.8) |
10.4 |
0.0013 |
|
Labor analgesia for suspected or confirmed COVID-19 |
7 (5.1) |
4 (3.6) |
3 (11.1) |
2.5 |
0.1108 |
The survey identified 16,791 cases (50.1%) of vaginal delivery, and 16,692 cases (49.9%) of caesarean delivery, which includes 1,565 intrapartum cesarean deliveries (8.5%, 1,565/18,356) converted from desired vaginal delivery (Table 2). We identified a total of 4,363 cases of epidural labor analgesia for labor with a labor analgesia rate of 26.0% (22.1% in general hospitals and 28.5% in women's hospital), including 485 intrapartum cesarean deliveries with epidural labor analgesia (31.0%, 485/1,565). As shown in Figure 2, the average labor analgesia rate in our survey at 26.0% showed a slight decrease as compared to monthly data from AQCC (32.2% in November 2019 and 28.2% in December 2019).
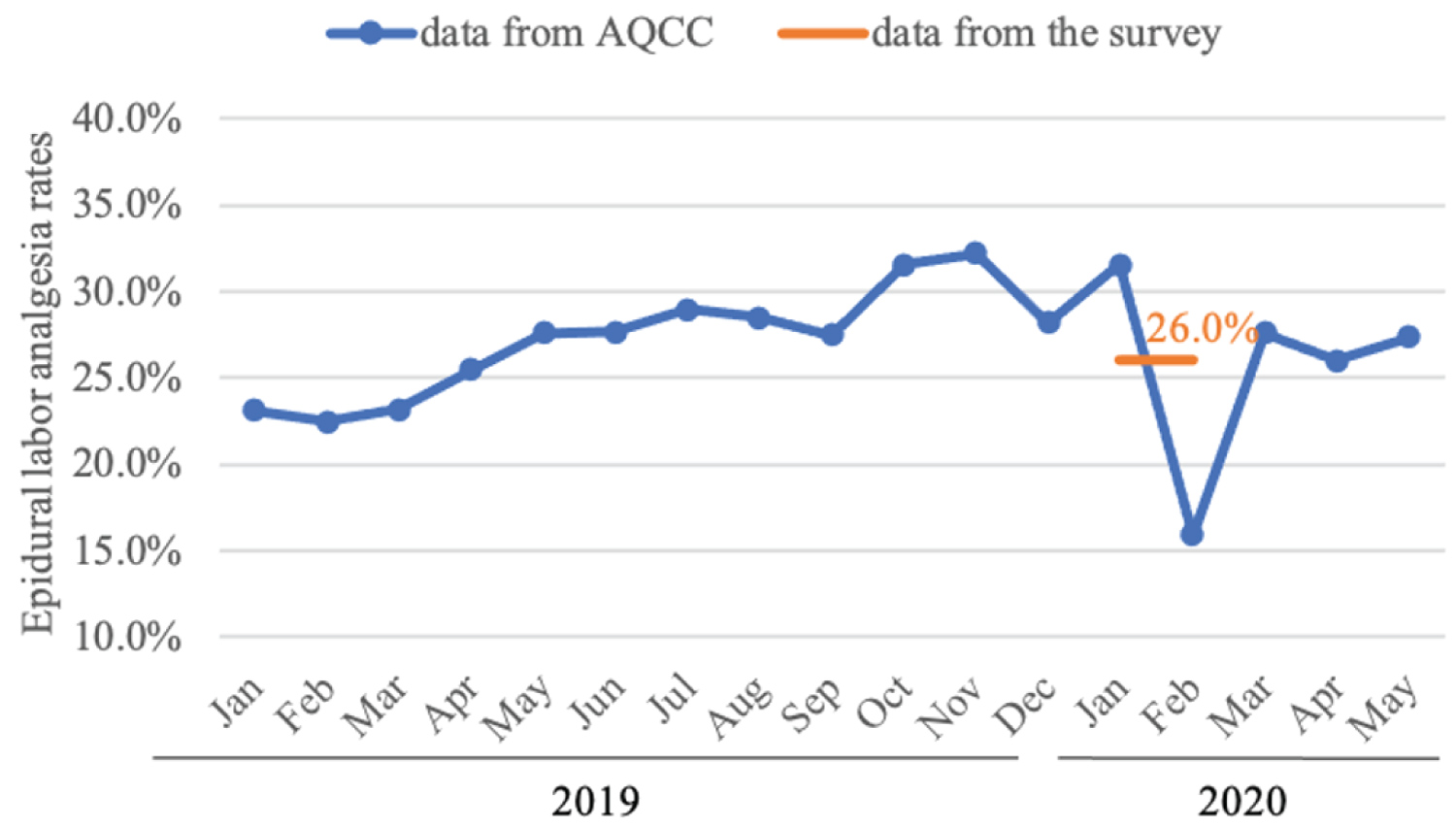
Figure 2:
Epidural labor analgesia rates from AQCC and the survey.
The monthly labor analgesia rates are from January 2019 to May 2020 from AQCC in Hubei, China, and the average labor analgesia rate are from January and February in 2020 from our survey.
Table 2: Obstetric care from January 1 to February 25 of 2020 in Hubei.
|
|
Total |
General hospital |
Women's hospital |
x2 |
p |
|
Labor and delivery |
|
|
|
|
|
|
Routine service for labor and delivery, hospitals |
108 |
82 |
26 |
|
|
|
Vaginal delivery, cases (%) |
16791 (50.1) |
6611 (44.2) |
10180 (54.9) |
125.87 |
< 0.0001 |
|
Caesarean delivery, cases (%) |
16692 (49.9) |
8330 (55.8) |
8362 (49.1) |
124.94 |
< 0.0001 |
|
Intrapartum cesarean deliveries converted from desired vaginal delivery, cases (%) |
1565 (8.5) |
877 (11.7) |
688 (6.3) |
78.68 |
< 0.0001 |
|
Labor analgesia |
|
|
|
|
|
|
Labor analgesia for routine labor and delivery, hospitals |
69 |
48 |
21 |
|
|
|
labor analgesia, cases (%1) |
4363 (26.0) |
1463 (22.1) |
2900 (28.5) |
77.84 |
< 0.0001 |
|
instrumental vaginal deliveries with labor analgesia, cases (%2) |
165 (3.8) |
111 (7.6) |
54 (1.9) |
79.81 |
< 0.0001 |
1Labor analgesia rate = Labor analgesia cases/vaginal delivery*100%; 2Instrumental vaginal deliveries with labor analgesia rate = Instrumental vaginal deliveries with labor analgesia cases/labor analgesia cases*100%
Characteristics, severity and outcomes of the infected patients
Table 3 shows that 83 COVID-19 cases were confirmed before or after surgery (68.6%, 83/121) and 38 suspected COVID-19 cases were excluded after surgery (31.4%, 38/121). Thus, the confirmed case rate over the whole period in parturients for caesarean delivery is estimated at around 497.24 per million people (83/16692). We did not seek information on acquired COVID-19 in patients for vaginal delivery since we do not have direct access to these data. Most caesarean delivery (97.5%, 118/121) was under epidural or spinal anesthesia. General anesthesia was performed only in three cases, including one suspected case that was excluded for infection after the surgery and two confirmed cases diagnosed before the surgery. For all the confirmed cases, post-operative isolation was performed. Neonatal asphyxia was observed in only one newborn among the confirmed COVID-19 pregnant women. All the newborns of suspected and confirmed cases had negative results of the nucleic acid test for SARS-CoV-2, and Apgar scores at 1 min and 5 min were all between 8 and 10.
Table 3: Perioperative information for the all cases with suspected or confirmed diagnosis of COVID-19.
|
|
Puerperas |
Infants |
|||||||
|
Case type |
Number (cases) |
Age (years) |
Gestational Week (weeks) |
Spinal or epidural/General anesthesia (cases) |
Postoperative isolation |
Apgar (1 min) |
Apgar (5 min) |
Dyspnea (cases) |
Discharge/ hospitalization (cases) |
|
Suspected cases excluded after surgery |
38 |
31.3 ± 4.0 |
37.0 ± 3.3 |
37/1 |
No |
8.1 ± 1.1 |
9.0 ± 0.9 |
5 |
33/5 |
|
Suspected case confirmed after surgery |
27 |
31.7 ± 5.2 |
38.0 ± 2.3 |
27/0 |
Yes |
9.0 ± 0.7 |
9.8 ± 0.5 |
1 |
26/1 |
|
Confirmed cases before surgery |
54 |
30.4 ± 4.0 |
38.1 ± 1.5 |
52/2 |
Yes |
8.7 ± 0.5 |
9.8 ± 0.5 |
0 |
42/12 |
Suspected cases are defined as presenting with a fever or any respiratory symptoms, especially in those with a history of travel to Wuhan or exposure to infected people within two weeks. Confirmed cases are defined as those who have symptoms and a positive viral test.
Among the 83 confirmed COVID-19 cases, only two patients were in critical condition (Table 4) and the rest of the cases had only mild to moderate symptoms. Of the critical patients, Patient 1 was transferred to the intensive care unit (ICU) afterwards and stayed in the ICU for one day before being transferred to an isolation ward. She was sent back to the ICU 6 days later due to respiratory failure and died on postoperative day 22.
Table 4: Perioperative information for the two cases with severe or critical condition of COVID-19.
|
Patient information |
Perioperative information |
Infants |
|||||||
|
Age |
Gestational Week |
Anesthesia method |
Anesthesia course |
Postoperative |
Outcome |
Apgar (1 min) |
Apgar (5 min) |
Health condition |
Nucleic Acid Test |
|
25 |
39 |
General |
Unstable |
ICU |
Died |
7 |
8 |
Heathy |
Negative |
|
27 |
36 + 5 |
Spinal |
Stable |
Isolation ward |
Recovered |
9 |
9 |
Heathy |
Negative |
Discussion
The survey included 33,483 cases from 138 hospitals in Hubei from January 1 to February 25 of 2020. The caesarean delivery rate was 49.9% and labor analgesia rate was 26.0%. Data reporting found 83 confirmed COVID-19 patients for caesarean delivery (0.50%) with the majority having had only mild to moderate symptoms and received epidural or spinal anesthesia without documented complications. No neonatal infection was detected.
Changes in obstetric anesthesia care at the early stage of pandemic
The caesarean delivery of 138 hospitals from our survey was 49.9% during the virus outbreak (55.8% in general hospitals and 49.1% in women's hospitals) which indicates a small increase. According to the "China Maternal and Child Health Care Development Report" (2019) issued by the National Health Commission, the average caesarean delivery rate in China was 36.7% in 2018. Considering the regional differences in mode of delivery in China, we checked the average caesarean delivery rate in Hubei Province in 2019, which was 48.6% (203,909/419,941, unpublished data from health commission of Hubei province). This small increase of caesarean delivery might be related to the expert consensus in China to limit labor and delivery length by relaxing the cesarean delivery indications [6].
Obstetric anesthesia care showed heterogeneous differences between general hospitals and women's hospitals. The 138-hospital survey showed that 26.1% of general hospitals (vs. only 3.7% in women's hospitals) temporarily stopped routine service for labor and delivery. More general hospitals did strict maternal triage, admission and isolation than women's hospitals, which might result in parturients switching to women's hospitals. Labor analgesia rates also showed heterogeneous difference between general hospitals and women's hospitals. Our survey showed a decrease of average labor analgesia rate at 26.0% (22.1% in general hospitals and 28.5% in women's hospitals). Only 5.1% (7/138) hospitals provided labor analgesia for COVID-19 patients. Early analgesia should be considered for these patients and the data clearly indicate that analgesia can be safely performed for such patients, furthermore epidural anesthesia can be used if intrapartum caesarean delivery is needed. There were 4.5% (1,565/18,356) intrapartum cesarean deliveries converted from desired vaginal delivery in the survey. The experience of labor analgesia in the women's hospitals could potentially be critical for those in the general hospitals in order to improve the labor analgesia across the country. Further study is needed.
Cause analysis for impact of COVID-19 on obstetric anesthesia
Obstetric clinics, especially parturients in the third trimester have a limited interval following admission, so any difficulties in treating with emergency obstetric anesthesia would significantly impact on the timely treatment and the anesthesia quality, which partly resulted in the low labor analgesia rate during January and February. The changes in admission including maternal triage, centralized quarantine or allocation to designated hospitals could delay the timely treatment. As shown in the survey, the maternal triage included fever clinics (89.9%), routine CT (53.6%), and mother and infant nucleic acid amplification test (40.6% and 29.7%). Those who have a suspected or confirmed diagnosis of COVID-19 are diverted to designated hospitals for COVID-19 patients. In our survey, the detection rate of cases confirmed before surgery is around 50%; therefore, many are confirmed after surgery.
Insufficient medical resources and medical staff might be associated with the low labor analgesia rate. In our survey, the under-equipped isolation or negative pressure wards (52.2%), isolation or negative pressure delivery rooms (27.2%) and isolation or negative pressure operating rooms (63.8%) would limit the proper medical care under the clinical challenges. Meanwhile, heavy workload of anesthesiologists would further worsen current medical care. Anesthesiologists in Hubei were allocated to assist other medical units during the outbreak, such as ICU (14.6%), isolation wards (8.8%) and fever clinics (8.0%), as shown in the survey.
Clinical severity and outcomes of confirmed patients and neonates
Most of the maternity patients with COVID-19 had only mild to moderate symptoms. Only two patients had severe symptoms. All the patients tolerated epidural or spinal anesthesia well, including the two patients with severe symptoms. The data on general anesthesia are very limited. While one patient with severe COVID-19 who had a caesarean delivery under spinal anesthesia later died, she had been discharged from the ICU a day after the procedure. It is unlikely that the anesthesia contributed a negative impact towards the outcome of this patient. But it is unclear also why most of the patients had only mild to moderate symptoms with a good prognosis. In this study, the overall infection rate for pregnant women is only around 0.50%, which might be due to the culture in China, where most pregnant women generally stay at home with limited social activities to be protected from the general population, and also all patients and family members voluntarily wear masks in public, including in hospitals.
A small-scale study indicated that vertical transmission of the virus cannot be ruled out [7]. Possible perinatal infection through the birth canal, lactation, and close contact after childbirth still needs attention. No neonatal infection was observed in this report.
Limitations of the study
This is a retrospective survey study and significant bias could potentially be introduced to the results. Since universal symptom survey and laboratory screen were widely available in Hubei after March, there might be ascertainment bias because of the shortage of testing in the early stage, which may in part result in the initial underestimating of the infection rates of patients in addition to a high false negative rate and asymptomatic patient population. Due to the clinical challenges and heavy workload at the early stage, many hospitals may be unwilling to report certain detailed information. In our survey, there were 81.2% of hospitals designated for COVID-19 patients and only 50.0% of hospitals offered routine service for labor and delivery. Thus, we may have underestimated some of the factors related to the findings. Reports of epidural and spinal anesthesia are collected together but the types are not distinguished in our survey. Further big data and multi-dimensional data analysis, may provide efficient and accurate data support for root-cause analysis.
Conclusions
General hospitals had a more significant decline of anesthesia care which might be due to reduction of obstetric services and timely admission because of maternal triage, insufficient medical resources and heavy workload of anesthesiologists. However, women's hospitals had shown higher capacity and quality of obstetric care but should still increase efforts with pandemic control on maternal triage, admission and isolation. Most of the infected patients had only mild symptoms with a good outcome. Epidural or spinal anesthesia and analgesia can be safely administered for patients with COVID-19. These findings may inform decision-making for anesthesia quality control in the epidemic stage.
Funding
National Key Research and Development Project (2018YFC2001805, PI, JW); Science and Technology Project in Hubei Province (2019ACA167, PI, SLY).
Acknowledgements
We thank all hospitals and anaesthesiologists who supported this study. We thank Prof. Renyu Liu from Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, PA, USA, for his help and guidance in study design and content edit. We thank Dr. Xin Huang and Mr. Qinghong Chen from the Department of Anesthesiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, for assisting in data collection.
Statement of the Manuscript
The manuscript has been read and approved by all the authors.
Conflict of Interests
None.
Author Contributions
JW, JJK and JW: Study design and data analysis; WMX, LYR, XY and RM: Data collection; JD, XDC and SLY: Study design and content edit.
References
- Bayefsky MJ, Bartz D, Watson KL. Abortion during the Covid-19 pandemic - Ensuring access to an essential health service. N Engl J Med. 2020 May 7;382(19):e47. doi: 10.1056/NEJMp2008006.
- Qiao J. What are the risks of COVID-19 infection in pregnant women? The Lancet. 2020 Mar 7;395(10226):760-2.
- Chen HJ, Guo JJ, Wang C, Luo F, Yu Xc, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet. 2020 Mar 7;395(10226):809-15.doi: 10.1016/S0140-6736(20)30360-3.
- Zhong Q, Liu YY, Luo Q, Zou YF, Jiang HX, Li H, et al. Spinal anesthesia for patients with coronavirus disease 2019 and possible transmission rates in anaesthetists: retrospective, single-centre, observational cohort study. Br J Anaesth. 2020 Jun;124(6):670-5. doi: 10.1016/j.bja.2020.03.007.
- Hu LQ, Flood P, Li Y, Tao W, Zhao P, Xia Y, et al. No Pain Labor & Delivery: A Global Health Initiative's Impact on Clinical Outcomes in China. AnesthAnalg. 2016 Jun;122(6):1931-8. doi: 10.1213/ANE.0000000000001328.
- National Center for Health Care Quality Management in Obstetrics.Suggestions on delivery management of pregnant women with COVID-19. Chin J ObstetGynecol, 2020,55(03): 150-2. DOI: 10.3760/cma.j.cn112141-20200224-00128
- Zeng H, Xu C, Fan J, Tang Y, Deng Q, Zhang W, et al.Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020 May 12;323(18):1848-9. doi: 10.1001/jama.2020.4861.