Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/169
Case Report | Volume 10 | Issue 1 Open Access
Anesthesia Management of Exit Procedure for Fetus with Mediastinal Teratoma: A Case Report
Deniz Kaya, MD1, Nedim Çekmen, MD, PhD1, Zeynep Ersoy, MD1 and Ender Fakioglu, MD2
1Department of Anesthesiology and Reanimation, Baskent University, Ankara, Turkey
2Department of Pediatric Surgery, Baskent University, Ankara, Turkey
Deniz Kaya, Department of Anesthesiology, Baskent University, Yukari Bahcelievler Maresal Fevzi Cakmak St. No: 45 Cankaya, Ankara 06490, Turkey, Tel: +90-3122126868/4867, E-mail: denizkaya398@gmail.comEditor: Renyu Liu, MD; PhD; Professor, Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, Center of Penn Global Health Scholar, 336 John Morgan building, 3620 Hamilton Walk, Philadelphia, PA 19104, USA, Fax: 2153495078, E-mail: RenYu.Liu@pennmedicine.upenn.edu
Received: January 29, 2023 | Accepted: February 20, 2023 | Published: February 23, 2023
Citation: Kaya D, Cekmen N, Ersoy Z, Fakioglu E. Anesthesia Management of Exit Procedure for Fetus with Mediastinal Teratoma: A Case Report. Transl Perioper Pain Med 2023; 10(1):505-507
Abstract
Development of prenatal diagnosis methods provides the opportunity for being prepared against the problems caused by congenital anomalies. The EXIT (Ex Utero Intrapartum Treatment) procedure makes possible to intervene in congenital anomalies that may cause ventilation and oxygenation problems in the fetus in the postnatal period. It requires careful preoperative preparation and a multidisciplinary team that includes perinatologists, neonatologists, pediatric surgeons and anesthesiologists. We aim to present the anesthesia management of an EXIT procedure for tube thoracostomy and intubation during cesarian section delivery of a fetus with an antenatal mediastinal mass and hydrops fetalis diagnosis, in the light of literature.
Keywords
Exit procedure, Anesthesia management, Multidisciplinary approach
Introduction
Modern imaging methods made it possible to diagnose early congenital anomalies in the prenatal period and to prevent the problems that these anomalies may cause. The procedures to be performed require thorough preoperative preparation and a multidisciplinary approach. The EXIT (Ex Utero Intrapartum Treatment) procedure is designed to intervene in cases in which the newborn is expected to lack adequate ventilation in the postnatal period. In this case report, we aim to present the anesthesia management of an EXIT procedure for tube thoracostomy and intubation during cesarian section delivery of a fetus with an antenatally mediastinal mass and non-immune hydrops fetalis (NIHF) diagnosis, in the light of literature.
Case Presentation
A 28-year-old woman, (gravida 1, para 0) at 31 weeks' gestation was referred to our clinic after adetailed antenatal ultrasound imaging revealed a mass in the mediastinum of the fetus. Fetal magnetic resonance imaging (MRI) revealed bilateral pleural effusion and a mass lesion in the anterior mediastinum, which was thought to originate from the right atrium (Figure 1). In the light of these findings the fetus was diagnosed with NIHF. It was decided to perform an EXIT procedure with bilateral tube thoracostomy and intubation. In the preoperative anesthesia examination of the mother, there was no additional systemic disease, ASA score was 2 and the patient's informed consent was obtained. In the operating room, after appropriate preoperative standard monitoring and positioning for left uterine displacement, the patient was intubated with rapid sequence induction without complications. Invasive arterial monitoring was carried out on the mother. Sevoflurane was administered at a MAC (Minimum Alveolar Concentration) value of 2.5-3.5 to ensure adequate depth of anesthesia and uterine relaxation. The mean arterial pressure (MAP) was kept above 65 mmHg for effective uteroplacental circulation, ephedrine and hydration were administered when hypotension occurred. After the newborn was delivered, bilateral tube thoracostomy was performed by pediatric surgeons without clamping the umbilical cord and the baby was intubated. During the EXIT procedure, the newborn's peripheral oxygen saturation has ranged between 85-90% and the procedure spanned 6 minutes in total. Approximately 10 mL of fluid drained from the right thoracostomy and 15 mL of fluid from the left. The newborn's APGAR score was evaluated as 6/8. The newborn was transferred to the neonatal intensive care unit (ICU) after the initial evaluation and essential treatments. Following the clamping of the umbilical cord, oxytocin was administered to the patient to prevent uterine bleeding. The approximate amount of bleeding of the mother during the operation was 250 mL and blood product transfusion was not required. After the incision was closed, the patient was extubated and transferred to the ward.
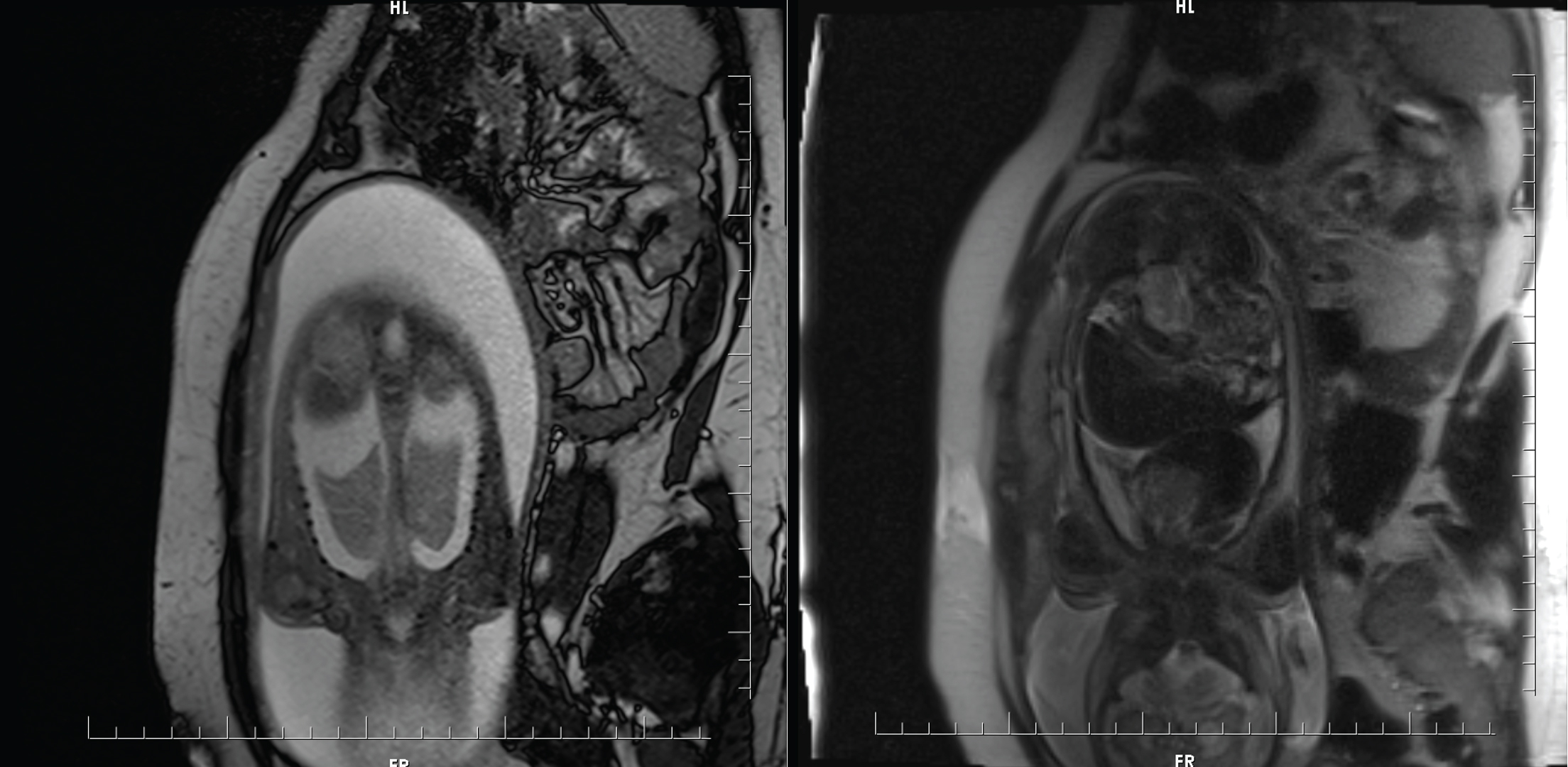
Figure 1: MRI section showing bilateral pleural effusion on the left, and a mass lesion in the anterior mediastinum on the right.
A sternotomy was performed on the newborn for mediastinal mass excision 7 days later. The mass was found to invade the heart and great vessels and had no clear borders, therefore the operation was terminated before the surgery could be performed. The biopsy result was consistent with immature teratoma. The newborn, who was being followed up in the ICU, died on the 19th day of follow-up due to obstructive shock because of the mass compression.
Discussion
Mediastinal teratomas are the second most common extragonadal teratomas in children [1]. These masses affect the mortality and morbidity of the newborn in the postnatal period, depending on the location of the mass, the effect of compression on the heart and major vessels, or the presence of NIHF. Cases of progressive prenatal pleural effusion associated with NIHF carry a high risk for fetal and neonatal death [2]. In our patient, NIHF developed due to a mediastinal teratoma. In order to ensure adequate ventilation and oxygenation of the newborn in the early postnatal period, the EXIT procedure was decided by the consensus of the neonatologist, pediatric surgeon, obstetrician and anesthesiologist.
The EXIT procedure allows interventions to be made to eliminate the ventilation problem of the newborn while the uteroplacental circulation continues. Fetal causes requiring EXIT procedure include cervical, mediastinal and lung masses, tracheal or laryngeal atresia that may cause airway obstruction [3].
The main goal in the EXIT procedure is to provide sufficient uteroplacental circulation throughout the process of fetal intervention without risking the mother and the fetus. For this reason, there are significant differences in anesthesia management from the standard c-section application. While preserving the uterine tone is aimed during the standard c-section, providing uterine relaxation in the EXIT procedure is a necessity to reduce the risk of placental separation and other possible risks [4]. The generally preferred method for sufficient uterine relaxation is the administration of inhalation anesthetics at x2 MAC in patients undergoing general anesthesia [5]. However, as a result of this uterine relaxation, the risk of uterine hemorrhage increases. Precautions should be taken for increased maternal bleeding risk, relevant blood and blood products should be prepared for the mother and fetus, and sufficient intravenous (IV) access should be provided. The high concentrations of inhalation anesthetics and the increased likelihood of bleeding can cause hypotension. Maternal MAP should be kept above 65 mmHg to ensure sufficient uteroplacental circulation. For this, adequate fluid volume resuscitation should be made and if necessary, vasopressors should be used. We also administered vasopressors when necessary to provide normotension in our case.
Neuraxial blocks with IV nitroglycerin administration can be considered as an alternative anesthesia method that can be used to provide uterine relaxation. This method can be preferred for short-term EXIT procedures where the risk of maternal bleeding is less [4,5]. Our case was also planned as a short-term procedure, so this alternative method could also be used, but we thought that high-dose sevoflurane administration under general anesthesia would be safer since the mother's anxiety and hemodynamic parameters could be better controlled, and it would be difficult to predict the duration of the surgical procedure.
Conclusion
In conclusion, proper application of the EXIT procedure can increase survival for the prenatally diagnosed anomalies that may cause postpartum ventilation and oxygenation problems. This requires a qualified multidisciplinary team in communication and adequate pre-operative arrangement. In addition to ensuring maternal-fetal safety during this procedure, the anesthesiologist should pay attention to providing sufficient uterine relaxation and uteroplacental circulation and keep in mind the increased bleeding risk.
Conflict of Interest
None.
References
- Barksdale EM, Obokhare I. Teratomas in infants and children. Curr Opin Pediatr. 2009;21(3):344-9.
- Cömert HSY, Kader S, Osmanagaoglu MA, Ural DA, Yasar ÖF, İmamoglu M, et al. Prenatal and Postnatal Management of Intrauterine Pleural Effusions Associated with Non immune Hydrops Fetalis. Am J Perinatol. 2022;39(13):1405-9.
- Garcia PJ, Olutoye OO, Ivey RT, Olutoye OA, Riou B. Case Scenario: Anesthesia for Maternal-Fetal Surgery. Anesthesiology. 2011;114(6):1446-52.
- Olutoye O. Anaesthesia for the EXIT procedure: A review. Southern African Journal of Anaesthesia and Analgesia. 2009;15(1):17-21.
- Kern C, Ange M, Morales M, Peiry B, Pfister R. Exutero intrapartum treatment (EXIT), a resuscitation option for intra-thoracic foetal pathologies. Swiss Med Wkly. 2007;