Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/178
Letter to the Editor | Volume 10 | Issue 3 Open Access
A Stratification and Team-Based Approach for the Management of Preoperative Hyperkalemia
Frank R Chen, MD1* and Jasper Han, BS2
1Department of Anesthesiology, Hospital of the University of Pennsylvania, Philadelphia, PA, USA
2University of Texas Southwestern Medical Center, Dallas, TX, USA
Frank R Chen, MD, Department of Anesthesiology, Hospital of the University of Pennsylvania, 3400 Spruce St, Philadelphia, PA 19103, USA, E-mail: Frankrxchen@gmail.comEditor: Li-Ming Zhang, MD, Associate Medical Director, UPMC-China, Associate Professor of Anesthesiology, Attending Anesthesiologist (Recertified), UPP Dept of Anesthesiology and Perioperative Medicine, 200 Lothrop Street, UPMC MUH Suite N-467, Pittsburgh, PA 15213, USA; Tel: 412-648-6077; Fax: 412-648-6014; Lab: 412-624-8386; Cell: 412-709-7617; E-mail: zhangl1@anes.upmc.edu
Received: May 28, 2023 | Accepted: October 23, 2023 | Published: October 26, 2023
Citation: Chen FR, Han J. A Stratification and Team- Based Approach for the Management of Preoperative Hyperkalemia. Transl Perioper Pain Med 2023; 10(3):543-545
Abstract
Hyperkalemia is a common electrolyte abnormality. There currently is no consensus on perioperative management of hyperkalemia. In this review we advocate for a stratification and team-based approach for the management of preoperative hyperkalemia.
Perioperative hyperkalemia is an electrolyte abnormality that is associated with cardiac disease, kidney disease, diabetes, and other systemic preoperative comorbidities [1]. Research has also identified clinical signs and symptoms of hyperkalemia, including progressive muscle weakness or paralysis [2,3] and classical peaked T waves and PR interval prolongation as well as other conduction abnormalities on electrocardiography (ECG). More recently, baseline hyperkalemia has been associated with increased likelihood of intraoperative and postoperative complications in orthotopic liver transplants [4]. Furthermore, it is known that patients with preoperative serum potassium levels greater than 5.5 mEq/L are twice as likely to require intraoperative management to address the hyperkalemia [5].
Despite our increasing understanding and even identification of the risks of hyperkalemia, there is a lack of evidence-based guidelines for management of preoperative hyperkalemia. One possible explanation for the lack of evidence-based guidelines is the variability of patient presentations along with the effects of hyperkalemia with other comorbidities. While electrocardiogram findings are suggestive of cardiac involvement, there may be no progression of abnormalities associated with increasing potassium levels and the absence of classical findings may not rule out conduction abnormalities secondary to hyperkalemia [6-8]. Common comorbidities, including CKD, often exacerbate hyperkalemia which, in return, is associated with progressively increased mortality risk when compounded with these comorbidities [2]. At the same time, other findings suggest that with CKD, particularly end stage renal disease, chronic hyperkalemia can lead to a theoretical protective effect against the electrophysiologic consequences of extreme hyperkalemia [9,10]. The unclear interaction of comorbidities and variability of patient presentation makes it difficult for clear recommendations on perioperative management strategies for patients with hyperkalemia.
Liu, et al. (2023) emphasized the need for evidence-based guidelines for management of hyperkalemia [11]. We agree with the aforementioned evidence-based guidelines. In addition to these guidelines, we advocate for a stratification and team-based approach to management of hyperkalemia with the following components:
First of all, (1) Stratification should be primarily dictated by ASA classification (I-VI) as well as surgical urgency of the case; emergent cases may often need to proceed regardless of potassium levels while elective cases can be rescheduled if necessary (Figure 1). (2) The surgery type should next direct stratification of cases. Procedures involving cardiac, vascular, or renal systems may be seen as high risk for patients with preoperative hyperkalemia compared to other low-risk types of procedures (melanoma, ocular, breast). In addition to procedures involving certain systems, any additional procedure with anticipated electrolyte or hemodynamic shifts such as transplant, endocrine, and neurosurgical procedures should also be viewed as high-risk. After consideration of surgery type, cases should be stratified by (3) medical comorbidities and degree of control over the comorbidities. Common ones to be considered here include chronic kidney disease, type 2 diabetes mellitus, liver disease, heart failure, chronic infections, and malignancies. As mentioned by Liu, et al., there should be consideration for intraoperative medical management of hyperkalemia via additional IV medications including calcium gluconate and insulin with glucose [11]. With all these factors dictating stratification in management, we finally stress the importance of (4) close communication between surgery, anesthesia, medicine, and all OR staff for patients with hyperkalemia in order to promote a unified approach to how and when to proceed.
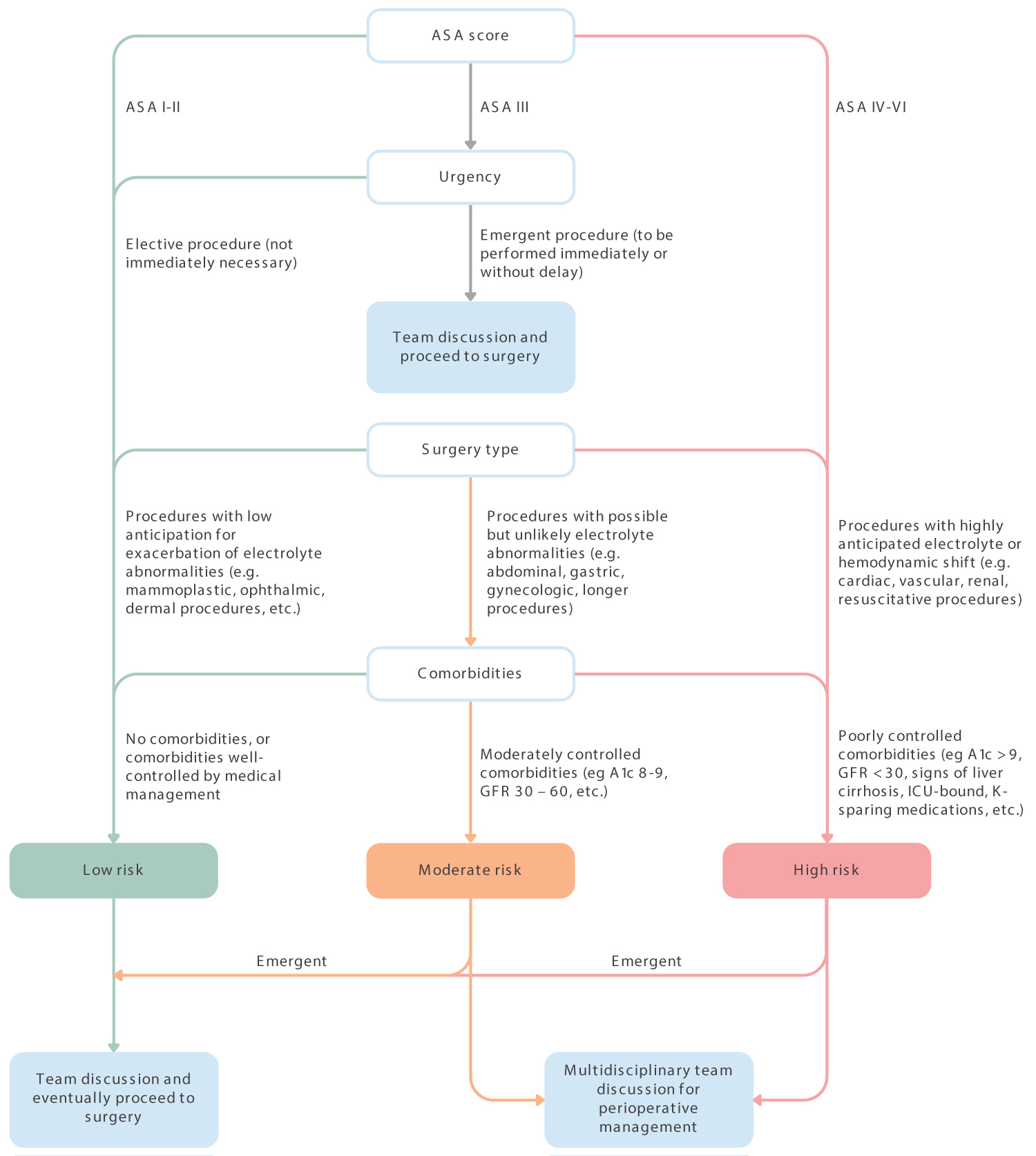
Figure 1: ASA classification (I-VI) as well as surgical urgency of the case.
References
- Collins AJ, Pitt B, Reaven N, et al. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46(3):213-221.
- Finch CA, Sawyer CG, Flynn JM. Clinical syndrome of potassium intoxication. Am J Med. 1946;1:337-352.
- Bell H, Hayes WL, Vosburgh J. Hyperkalemic paralysis due to adrenal insufficiency. Arch Intern Med. 1965;115:418-420.
- Xia VW, Ghobrial RM, Du B, et al. Predictors of hyperkalemia in the prereperfusion, early postreperfusion, and late postreperfusion periods during adult liver transplantation. Anesthesia & Analgesia. 2007;105(3):780-785.
- Zaki KS, Majid U, Islam N. Spurious hyperkalaemia: an insight. J Pak Med Assoc. 2011;61(3):297-299.
- Aslam S, Friedman EA, Ifudu O. Electrocardiography is unreliable in detecting potentially lethal hyperkalaemia in haemodialysis patients. Nephrol Dial Transplant. 2002;17(9):1639-1642.
- Khattak HK, Khalid S, Manzoor K, Stein PK. Recurrent life-threatening hyperkalemia without typical electrocardiographic changes. J Electrocardiol. 2014;47(1):95-97.
- Martinez-Vea A, Bardaji A, Garcia C, Oliver JA. Severe hyperkalemia with minimal electrocardiographic manifestations: a report of seven cases. J Electrocardiol. 1999;32(1):45-49.
- Surawicz B, Chlebus H, Mazzoleni A. Hemodynamic and electrocardiographic effects of hyperpotassemia. Differences in response to slow and rapid increases in concentration of plasma K. Am Heart J. 1967;73(5):647-664.
- Ahmed J, Weisberg LS. Hyperkalemia in dialysis patients. Semin Dial. 2001;14(5):348-356.
- Liu H, Tong Y. A Call for an evidence-based guideline for the perioperative management of hyperkalemia. Translational Perioperative and Pain Medicine. 2023;10(1).