Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/187
Case discussion | Volume 11 | Issue 2 Open Access
Stellate Ganglion Block for Persistent Hiccups Secondary to Lumbar Transforaminal Epidural Steroid Injection: A Case Discussion
Fatemeh Nazari, MD1* and Artadokht Khoshooei, MD2
1Fellowship of Interventional Pain Management, Pain Clinic, Naja Vali-Asr General Hospital, Tehran, Iran
2Associate Professor, Fellowship of Interventional Pain Management, Department of Pain Management, Faculty of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Fatemeh Nazari, MD, Fellowship of Interventional Pain Management, Pain Clinic, Naja Vali-Asr General Hospital, Tehran, Iran, Tel: +98-9123761344, E-mail: F.nazari1983@yahoo.comEditor: Renyu Liu, MD; PhD; Professor, Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, Center of Penn Global Health Scholar, 336 John Morgan building, 3620 Hamilton Walk, Philadelphia, PA 19104, USA, Fax: 2153495078, E-mail: RenYu.Liu@pennmedicine.upenn.edu
Received: May 31, 2024 | Accepted: July 27, 2024 | Published: August 03, 2024
Citation: Nazari F, Khoshooei A. Stellate Ganglion Block for Persistent Hiccups Secondary to Lumbar Transforaminal Epidural Steroid Injection: A Case Discussion. Transl Perioper Pain Med 2024; 11(2):606-611
Abstract
Epidural steroid injections (ESIs), can cause persistent hiccups in rare cases. In the literature, the most frequently implicated drug group associated with hiccups is the corticosteroid class, even though there is no clear understanding of the underlying etiology, after a lumbar transforaminal epidural block using dexamethasone for lumbar radiculopathy, a 40-year-old man presented with persistent hiccups. During the eighth day following injection, in the absence of improvement with medications such as gabapentin, baclofen, metoclopramide, and chlorpromazine, a stellate ganglion block (SGB) was carried out. The frequency of hiccups began to decrease, and one hour later, they completely disappeared. At follow-up appointments, there had been no recurrence of hiccups for him. Stellate ganglion block may be an effective treatment option for medically refractory patients, according to this study.
Keywords
Persistent hiccups, Epidural steroid injection, Lumbar transforaminal block, Dexamethasone, Stellate ganglion block
Introduction
It is common to perform interventional spine procedures in order to relieve acute or chronic pain [1]. The treatment usually involves the use of corticosteroids and local anesthetic combinations. Although patients may experience temporary and minor complications during these procedures, these procedures are generally considered safe [2]. Several studies have shown that epidural steroid injections are associated with hiccups. It is important to note that persistent hiccups, which are Over 48 hours in duration, are generally benign and self-limited, but can result in a great deal of distress, sleep disorders, exhaustion, fatigue, depression, and malnutrition. The treatment of hiccups has been accomplished through the use of a variety of pharmacological and non-pharmacological interventions. Hiccups caused by surgical procedures, strokes, abdominal organ damage, and central nervous system pathology can be effectively treated with the stellate ganglion (SG) block [1,3]. In this report, we aim to describe a case of persistent hiccups following lumbar epidural steroid injection in a 40-year-old male patient suffering from chronic radicular back pain as a result of disc protrusion in the L4-L5 disc.
Case Discussion
The patient is a 40-year-old male who presented to the pain clinic with chronic low back pain that was not responding to analgesics and physical therapy. The physical examination revealed that he was suffering from low back pain, numbness in the left lower extremity, and left-sided lower extremity pain. In an MRI scan, it was noted that the L4-L5 disc was protruding in the central and left foraminal regions. He underwent a fluoroscopically guided, left L4, transforaminal epidural steroid injection. During the procedure, the patient was placed prone. Under local anesthesia with 2 mL of 1% lidocaine without epinephrine, a 22-gauge spinal needle was used for the injection of 8 mg dexamethasone and 4 mg rupivacaine into the lumbar transforaminal epidural space, at the level of L4-L5 on the left side. Due to a safer clinical outcome and no inferior efficacy profile, a non-particulate steroid was used in the treatment of our patient.
There were no bleeding or neurological complications following the procedure and no changes in the patient's vital signs. Approximately two hours following the procedure, the patient was discharged from the clinic.
The following day, the patient presented us with a clinical picture of hiccups, causing him to lose sleep and feel fatigued. Approximately six hours after the epidural injection, the patient began experiencing mild hiccups that did not coincide with any other symptoms. A gradual increase in the frequency of the hiccups was observed over time. It was recommended to treat the patient with 10 mg baclofen twice a day and 300 mg gabapentin every eight hours, but the clinical condition did not improve within the next five days. As well, intravenous chlorpromazine, metoclopramide, and omeprazole were not effective in improving the patient's condition.
During the eighth day following the epidural steroid injection, we decided to perform an ultrasound-guided right-sided stellate ganglion block due to its higher safety profile (lower risk of hitting the thoracic duct and pneumothorax). An in-plane approach was used for the injection of 4 mL of 0.2% ropivacaine using a 25-gauge spinal needle. Immediately following the procedure, Horner syndrome occurred on the right side (miosis and ptosis) indicating that the SGB was successful. Furthermore, the patient experienced hoarseness as a result of recurrent laryngeal nerve block. In the hour following the procedure, the patient's hiccups gradually decreased in frequency and duration, and one hour after the block, he eventually did not hiccup anymore. At follow-up appointments, one week, one month, and 3 months after the procedure, he did not experience any recurrence of hiccups.
Discussion
As a reflex, an unexpected spasm of the diaphragm has caused hiccups, which leads to the inspiratory muscle contraction, and it is followed by a sudden glottis closure. There is not a clear understanding of the pathophysiology of hiccups [5,6].
Figure 1 illustrates the anatomy and overall pathophysiology of hiccups. In the hiccups reflex arc, there are three components: The afferent limb, the Central processing unit, and the Efferent limb. An afferent limb consists of a phrenic nerve, vagus nerve, and sympathetic chain originating from T6 to T12 thoracic segments. Initially, the phrenic nerve is considered a unique efferent limb in the hiccups reflex (nerves to diaphragm), but further efferent limbs to the glottis (via the recurrent laryngeal nerve), intercostal muscles (via the T1 to T11 intercostal nerves) and scalene muscles (via the plexal branches C5-C7), are also suspected to be involved [6]. There is an unspecified anatomic site between cervical C3 to C5 segments and the brain stem that is responsible for the central link between afferent and efferent pathways of the hiccups reflex. A number of neurotransmitters are involved in the processing of information, including gamma-aminobutyric acid (GABA) and dopamine [6]. These neurotransmitters can regulate the central mechanism.
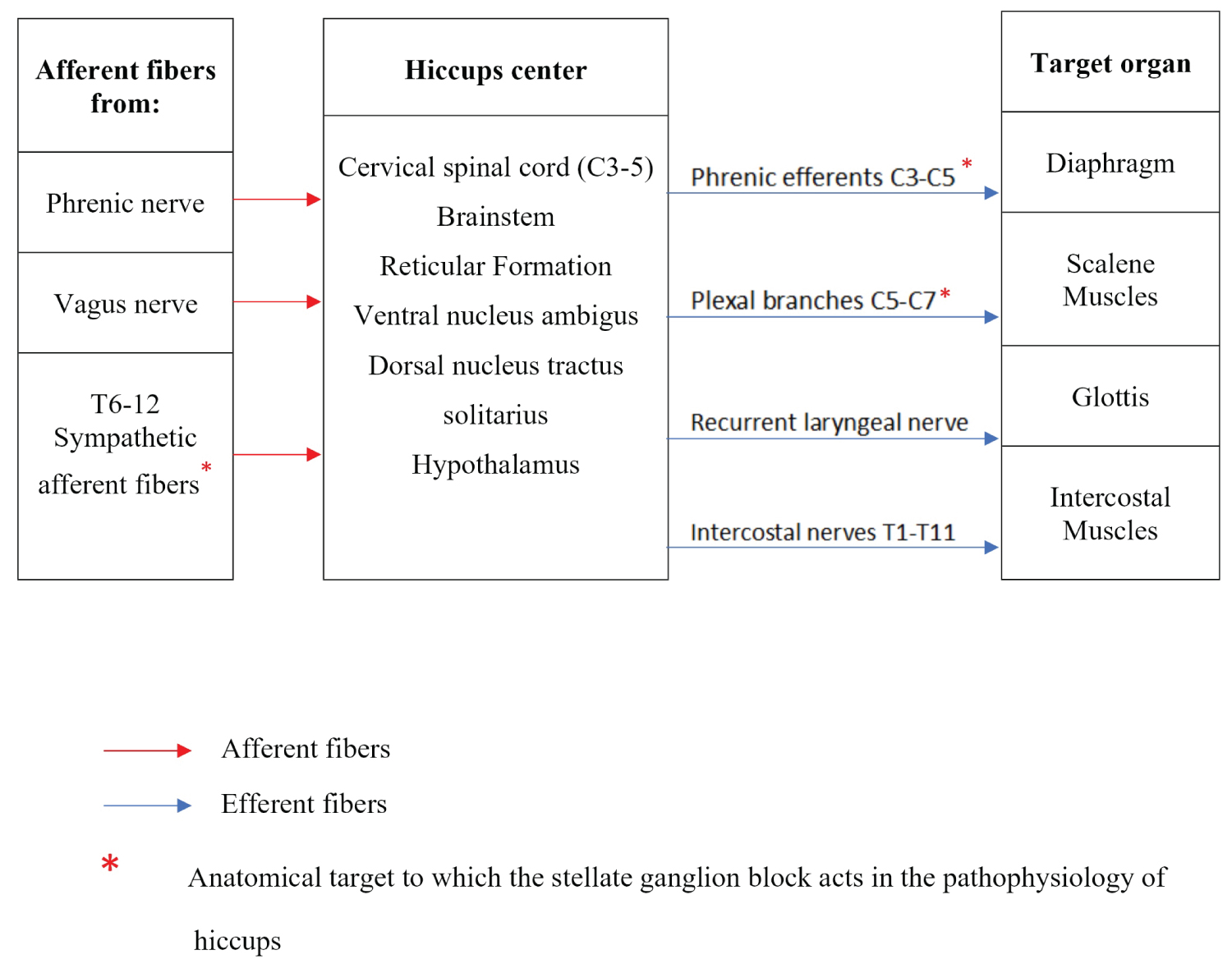
Figure 1:
The putative hiccups reflex arc. It includes the afferent limb to receive stimulation either located in the central nervous system or from peripheral lesions, central brain processing, and the efferent limb to convey responded signals to the diaphragm (via the phrenic nerve), glottis (via the recurrent laryngeal nerve), intercostal muscles (via the T1 to T11 intercostal nerves) and scalene muscles (via the plexal branches C5-C7). Hiccups are the sudden onset of diaphragmatic and intercostal muscle contraction and are immediately followed by laryngeal closure. Sudden closure of the glottis results in the "hic" sound.
Stellate ganglion block has an inhibitory effect on the sympathetic afferent limb and the efferent limb of the hiccups reflex arc, which includes the phrenic nerve (C3-C5) and innervation to the anterior scalene muscle (C5-C7).
Hiccups are classified based on their duration as transient hiccups (minutes or seconds in duration), persistent hiccups (over 48 hours in duration), or intractable hiccups (more than one month in duration) [7]. Hiccups most often result from idiopathic causes, but a variety of organic and psychological causes have been identified as well. Most organic hiccups are caused by problems with the gastrointestinal system (Table 1). It is known that a number of pharmacologic agents can cause hiccups, including steroids (Table 2) [8].
Table 1: Causes of persistent hiccups (according to the recommendations of Arjang Abbasi, et al., Daniel J Lopez, et al., and Chang FY, et al. [1,3,8]).
|
Disorders of the central nervous system |
Vascular (Ischemic or hemorrhagic stroke, Arteriovenous malformations, Giant cell arteritis) Central nervous system infections Structural (Head trauma, Intracranial neoplasms) |
|
Vagus or phrenic nerve involvement |
Goiter Pharyngitis, Laryngitis, Irritation of the tympanic membrane Neck cyst or tumor |
|
Gastrointestinal disorders |
Esophagitis or Gastritis, Esophageal or Gastric carcinoma, Peptic ulcer disease Pancreatitis, Pancreatic cancer Hepatitis, Gallbladder disease Inflammatory bowel disease, Bowel obstruction |
|
Thoracic disorders |
Enlarged lymph nodes (infection or neoplasm) Pulmonary and mediastinal infections or tumors Chest trauma |
|
Cardiovascular disorders |
Myocardial infarction, Pericarditis, Aortic aneurysms |
|
Toxic or metabolic disorders |
Herpes zoster, Influenza, Tuberculosis, Malaria Alcohol, Diabetes mellitus Uremia, Hypocalcemia, Hyponatremia, Hypocapnia |
|
Disorders due to surgery or anesthesia |
Neck extension (stretching of phrenic nerve) Intubation (stimulation of glottis) and general anesthesia Epidural injections Traction on viscera |
|
Psychogenic |
Anorexia nervosa, Malingering, Stress, Excitement Conversion reaction, Schizophrenia |
|
Drugs |
Listed in Table 2 |
Table 2: Drugs possibly associated with triggering hiccups [1,3,8].
|
Steroids |
Betamethasone, Dexamethasone, Hydrocortisone, Methylprednisolone, Prednisolone, Triamcinolone, Oxandrolone, Progesterone |
|
Benzodiazepines |
Midazolam, Lorazepam |
|
Anesthetics |
Barbiturates, Bupivacaine, Etomidate, Ketamine, Propofol |
|
Antibiotics |
Amoxicillin, Azithromycin, Cefotetan, Ceftriaxone, Doxycycline, Clarithromycin, Imipenem/Cilastatin, Ofloxacin, Pentamidine, Sulfonamides, Trimethoprim/Sulfamethoxazole |
|
Central nervous system agents |
Anticonvulsants (Ethosuximide) Anti-depressants (Fluvoxamine, Paroxetine) Antipsychotics (Clozapine, Perphenazine) Benzodiazepines (Chlordiazepoxide, Diazepam, Midazolam) Dopamine agonists (Levodopa, Pergolide, Pramipexole) |
|
Opioids |
Hydrocodone, Morphine |
|
Chemotherapeutic agents |
Platinum, Cyclophosphamide, Taxanes, Vinca Alkaloids, Topoisomerase inhibitors, Gemcitabine |
|
Miscellaneous |
Ketotifen, Magnesium, Megestrol acetate, Nicotine gum |
Table 3: Drugs used in the management of hiccups [7].
|
Drug |
Dose |
|
Baclofen |
5 mg twice per day maximum dose: 75 mg/day |
|
Metoclopramide |
Oral: 5-10 mg, 3 or 4 times/day up to 80 mg daily 10 mg IV/IM |
|
Chlorpromazine |
Oral: 12.5-50 mg every 4-6 hours, May also be given intramuscularly or intravenously |
|
Gabapentin |
900-1200 mg daily, dosed 3 times daily |
|
Haloperidol |
2-10 mg daily |
|
Olanzapine |
2.5-10 mg daily, as 1 or 2 doses |
The effects of corticosteroids can be described as stimulating the hiccups reflex arch and lowering the threshold for synaptic transmission in the midbrain. It has been reported that oral, intramuscular, and intravenous administration of corticosteroids may be responsible for the etiology of hiccups. Steroid-induced hiccups are commonly caused by dexamethasone. As opposed to other steroid drugs, dexamethasone shows a distinctive morphology and affinity for receptors of hiccups reflex in the brain stem [9].
Multiple cases of hiccups have been reported by MacGregor, et al. with a variety of steroid injections, as well as peripheral intra-articular injections, injections in subacromial bursa, iliopsoas bursa, plantar fascia, and lateral epicondyle [1]. It has been reported in the literature that many cases of hiccups have occurred following cervical/thoracic [6]/lumbar [10]/caudal ESIs [11], facet and Sacroiliac joint injections, which resolved spontaneously [10] or with the use of medication such as baclofen, gabapentin or chlorpromazine [11]. In these circumstances, hiccups may result from changes in the balance between cerebrospinal fluid volume and compression of the dural sac due to the solution's volume, as a result of injection into an epidural space [12]. In upper lumbar and thoracic ESIs, the injectate can reach the sympathetic afferent chain between T6 and T12, which initiates the hiccups reflex [6]. In our study, as a result of confirmatory fluoroscopic guidance, the injected solution did not reach this area.
A controversial association exists between local anesthetics and hiccups. The use of bupivacaine and levobupivacaine, which are local anesthetics, has been identified as causing hiccups in a few reports to date [5]. Additionally, local anesthetics have been shown to be an effective treatment for persistent hiccups that are refractory to other treatments [13]. Intractable or persistent hiccups may be treated by intravenous or nebulized lidocaine [1].
Nonpharmacologic treatment options include drinking cold water and keeping one’s breath in order to cause disruption of vagal afferents in the hiccups reflex arc. In addition, the maneuver of Valsalva and the massage of the carotid artery can be effective in absolving hiccups through the stimulation of the vagal nerve [14].
A variety of medications can be used to treat hiccups, including dopamine-altering drugs such as chlorpromazine, metoclopramide, and baclofen, antipsychotic drugs such as olanzapine, GABA-altering drugs such as gabapentin, and proton pump inhibitors such as omeprazole for gastroesophageal reflux disease (Table 3) [7].
Nerve-blocking procedures like phrenic nerve blocks [15,16] and surgical treatments may be recommended if these remedies prove ineffective. Hiccups can be effectively managed by Stellate ganglion block (SGB) as a complementary treatment [3,7]. The stellate ganglion (also known as the cervicothoracic ganglion), is formed by the inferior cervical ganglion and the superior thoracic ganglion. There is no clear understanding of how SGB works in patients with persistent hiccups, but a few possible mechanisms can be proposed. In the first instance, SGB may have an inhibitory effect on the sympathetic afferent limb in the hiccups reflex arc, thereby alleviating the symptoms [17]. Thoracic sympathetic nerve fibers originate from the spinal cord and through the cervicothoracic ganglion, the impulses are transmitted to the brain, and this path may have been obstructed by SGB [18]. There are similarities between this mechanism used for blocking the afferent limb of the hiccups reflex arc with a thoracic epidural block. As a second possibility, as a result of SGB, the arc of the hiccups reflex may have been affected, thus alleviating symptoms. During acute or chronic stress, nerve growth factor (NGF) levels increase in the brain. The NGF diffuses backward to the stellate ganglion where it stimulates the growth of sympathetic nerve terminals. As a result, norepinephrine (NE) levels in the brain increase, causing a variety of diseases. It is thought that SGB counteracts this mechanism by reducing the levels of both NGF and NE in the body, thereby alleviating the symptoms. It is believed that this mechanism contributes to the effectiveness of acupuncture in treating hiccups. With acupuncture, patients who suffered from persistent hiccups showed altered secretion patterns of serotonin, norepinephrine, and gamma-aminobutyric acid (GABA), in the brain [8]. A third possibility is that SGB probably affected the efferent limb of the hiccups reflex arc, which includes the phrenic nerve (C3-C5) and innervation to the anterior scalene muscle (C5-C7). There is a connection between sympathetic nerve trunks in the stellate ganglion, and spinal nerves, which are as gray rami communicantes. As a result, blockades of this ganglion have the potential to affect the innervation of the anterior scalene and phrenic nerve that connects to the spinal nerve (Figure 1) [19,20].
In a patient with motor vehicle collision (MVC), Daniel J Lopez, et al. reported a prolonged cessation of hiccups using ultrasound-guided stellate ganglion blocks [3].
In a study by Ran Lee, et al., three patients who experienced persistent hiccups in the first three days following abdominal surgery, were cured with an SGB. Hiccup intensity and frequency reduced as a consequence of the procedure and then completely disappeared after the procedure [7].
Because most cases of hiccups resolve spontaneously, they are benign and self-limiting. They may, however, be very disturbing at times. It is important for a clinician to be familiar with the detrimental effects that persistent hiccups can have in terms of the life quality of a patient. If necessary, their responsibility is to offer a comprehensive and active treatment program. There is a need for extensive research on this subject in order to understand the underlying causes and to determine whether treatment is necessary. It has been found that there is no statistical significance between medications and resolution, and it may also be a matter of chance that the hiccups resolved after the medication. There is still a lack of understanding regarding the causes and consequences of persistent hiccups following epidural steroid injections. At this point, no direct correlation can be established between hiccups following epidural injection and patient age and ethnicity, site of injection, or composition of injection. In order to develop a protocol for treating hiccups following epidural steroids, further studies should be conducted in systematic reviews or meta-analyses.
There should be additional studies conducted to identify the underlying mechanisms of action of SGB. In spite of this, the technique is a simple, safe, and efficient approach for treating persistent hiccups, which may be used alongside other treatments.
As indicated in the case report, and other cases, it would be reasonable to include this potential complication in the consent form in order to inform patients before similar procedures are performed.
Acknowledgment
The authors would like to thank the medical staff in the pain clinic at Valiasr General Hospital for their support. Also, we thank the patient and his family who participated in this study.
Funding
This research received no specific grant from any funding agency in the public or commercial.
Conflict of Interest
The authors further declare that they have no conflict of interest.
Ethical Approval
This case report study did not strictly meet the criteria of research and did not need IRB approval. Written informed consent was obtained from the patient for publication.
References
- Abbasi A, Roque-Dang CM, Malhotra G. Persistent hiccups after interventional pain procedures: A case series and review. Journal of the American Academy of Physical Medicine and Rehabilitation. 2012;4(2):144-151. | DOI: 10.1016/j.pmrj.2011.09.005.
- Ghasemi M, Taheri M, Nazari F, Khoshooei A, Amanollahi A, et al. Comparison of ultrasound-guided local dexmedetomidine injection vs corticosteroid injection in the treatment of chronic plantar fasciitis: A randomized clinical trial. Novelty in Biomedicine. 2023;11(3):122-130. | DOI: 10.22037/nbm.v11i3.41828.
- Lopez DJ, Kumar S. Stellate ganglion block for intractable hiccups secondary to a motor vehicle collision. Cureus Journal of Medical Science. 2023;15(4):e37030. | DOI: 10.7759/cureus.37030.
- Stacey SK, Bassett MS. Hiccup relief using active prolonged inspiration. Cureus Journal of Medical Science. 2024;16(1):e53045. | DOI: 10.7759/cureus.53045.
- McAllister RK, McDavid AJ, Meyer TA, Bittenbinder TM. Recurrent persistent hiccups after epidural steroid injection and analgesia with bupivacaine. Anesthesia and Analgesia. 2005;100(6):1834-1836. | DOI: 10.1213/01.ANE.0000153016.82444.20.
- Slipman CW, Shin CH, Patel RK, Braverman DL, Lenrow DA, et al. Persistent Hiccups Associated With Thoracic Epidural Injection. American Journal of Physical Medicine and Rehabilitation. 2001;80(8):618-621. | DOI: 10.1097/00002060-200108000-00014.
- Lee AR, Cho YW, Lee JM, Shin YJ, Han IS, et al. Treatment of persistent postoperative hiccups with stellate ganglion block: Three case reports. Medicine. 2018;97(48):e13370. | DOI: 10.1097/MD.0000000000013370.
- Chang FY, Lu CL. Hiccups: Mystery, nature and treatment. Journal of Neurogastroenterology and Motility. 2012;18:123-130. | DOI: 10.5056/jnm.2012.18.2.123.
- Iijima M, Uchigata M, Ohashi T, Kato H. Intractable hiccups induced by high-dose intravenous methylprednisolone in a patient with multiple sclerosis. European Journal of Neurology. 2006;13:201-202. | DOI: 10.1111/j.1468-1331.2006.01097.x.
- Karthik A, Kaur P, Noufin S, Beegum S. Persistent hiccups as a potential complication after interlaminar epidural steroid injection should be included in the consent form: A case discussion. Translational Perioperative and Pain Medicine. 2022;9(2):449-451. | DOI: 10.31480/2330-4871/157.
- Kaydu A, Kılıç ET, Gökçek E, Akdemir MS. Unexpected complication after caudal epidural steroid injection: Hiccup. Anesthesia Essays and Researches. 2017;11(3):776-777. | DOI: 10.4103/aer.AER_90_17.
- Higuchi H, Adachi Y, Kazama T. Effects of epidural saline injection on cerebrospinal fluid volume and velocity waveform: A magnetic resonance imaging study. Anesthesiology. 2005;102:285-292. | DOI: 10.1097/00000542-200502000-00008.
- Kim JE, Lee MK, Lee DK, Choi SS, Park JS. Continuous cervical epidural block: Treatment for intractable hiccups. Medicine. 2018;97(6):e9444. | DOI: 10.1016/j.ejon.2018.10.005.
- Cole JA, Plewa MC. Singultus. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538225.
- Rangel GW, Agón KO, Santos DR, Duran JP, Diaz KNC. Ultrasound-guided bilateral pulsed radiofrequency of the phrenic nerve for prolonged hiccups: A Case Report. Pain. 2023;13(7):379-384. | DOI: 10.2217/pmt-2023-0008.
- Ke X, Wu Y, Zheng H. Successful termination of persistent hiccups via combined ultrasound and nerve stimulator-guided singular phrenic nerve block: A case report and literature review. Journal of Medical Internet Research. 2023;51(12):1-7. | DOI: 10.1177/03000605231216616.
- Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician. 2000;3:294-304.|DOI: 10.36076/ppj.2000/3/294.
- Mulvaney SW, McLean B, de Leeuw J. The use of stellate ganglion block in the treatment of panic/anxiety symptoms with combat-related post-traumatic stress disorder; preliminary results of long-term follow-up: A Case Series. Pain Practice. 2010;10:359-365. | DOI: 10.1111/j.1533-2500.2010.00373.x.
- Lipov EG, Joshi JR, Sanders S, Slavin KV. A Unifying theory linking the prolonged efficacy of the stellate ganglion block for the treatment of chronic regional pain syndrome (CRPS), hot flashes, and post-traumatic stress disorder (PTSD). Medical Hypotheses. 2009;72:657–661. | DOI: 10.1016/j.mehy.2009.01.009.
- Glick DB, Miller RD, Cohen NH, Eriksson LI. The autonomic nervous system. Miller's Anesthesia 8th edition. Philadelphia: Churchill Livingstone/Elsevier. 2015:346-386.