Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/211
Case Report | Volume 12 | Issue 1 Open Access
Unilateral Modified Radical Mastectomy with Paravertebral Block Under Remifentanil Sedation in a Pemphigus Vulgaris Patient with Multiple Comorbidities: A Case Report
Nursultan Akmatov1, İrem Yıldız1,* , Nedim Çekmen1 and Sedat Yıldırım2
1Başkent University Ankara Hospital, Department of Anesthesiology and Reanimation
2Başkent University Ankara Hospital, Department of General Surgery
İrem Yıldız, MD, Baskent University, Faculty of Medicine, Department of Anesthesiology and Intensive Care Unit, Ankara, TurkeyEditor: Renyu Liu, MD; PhD; Professor, Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, Center of Penn Global Health Scholar, 336 John Morgan building, 3620 Hamilton Walk, Philadelphia, PA 19104, USA, Fax: 2153495078, E-mail: RenYu.Liu@pennmedicine.upenn.edu
Received: Apr 25, 2025 | Accepted: Dec 20, 2025 | Published: Dec 24, 2025
Citation: Akmatov N, Yıldız I, Çekmen N, et al. Unilateral Modified Radical Mastectomy with Paravertebral Block Under Remifentanil Sedation in a Pemphigus Vulgaris Patient with Multiple Comorbidities: A Case Report. Transl Perioper Pain Med 2025; 12(2):802-806
Abstract
Anesthesia management in patients with pemphigus vulgaris (PV) and multiple comorbidities is highly challenging for the anesthesiologist.We aimed to present anesthesia management with remifentanil sedation accompanied by thoracic paravertebral block (TPVB) in an 81-year-old high-risk patient with pemphigus vulgaris (PV) and multiple comorbiditieswho was planned for modified radical mastectomy (MRM). We suggest that TPVB can be used combined with sedation as an effective, safe, and feasible method for hemodynamic stability in intraoperative and postoperative pain control in patients undergoing MRM surgery and in reducing the need for postoperative analgesic use and perioperative complications.
Keywords
Pemphigus vulgaris, Multiple comorbidities, Modified radical mastectomy, Thoracic paravertebral block, Sedation
Introduction
Pemphigus vulgaris (PV) is a rare autoimmune condition caused by autoantibodies against desmoglein 1 and 3 proteins. Desmoglein 1 and 3 are intercellular junction proteins expressed in the skin, hair follicles, oral and pharyngeal mucosa, oesophageal mucosa, and external genital tract mucosa. These antibodies destroy intercellular connections in the epithelium, causing the mucosa to be sensitive to physical stress (Nikolski's sign) and causing painful blisters and erosions [1]. These pathologies are highly challenging for the anaesthesiologist in the perioperative periods [2].
Oral intake is reduced in these patients due to dysphagia due to PV. Accordingly, malnutrition, dehydration, electrolyte abnormalities, cachexia, hypoproteinemia, and hypoalbuminemia may develop. As a result, it increases the risk of complications, morbidity, and mortality in the perioperative period due to delayed wound healing, altered drug pharmacokinetics, delayed mobilization, and poor performance during the discharge and rehabilitation period [1, 2]. Airway management and mask ventilation can be complicated by oral and buccal scars that prevent adequate mouth opening and mobility of the tongue and pharynx. In addition, any airway intervention, including mask ventilation, oropharyngeal and supraglottic airway placement, and laryngoscopy, should be done with extreme caution as it can lead to infected and painful wounds that take a long time to heal [2].
Oncologic breast surgeries vary from simple palliative procedures to modified radical mastectomy (MRM) with axillary cleansing. General anesthesia (GA) is the most commonly preferred in these surgeries. Still, alternative regional anesthesia (RA) techniques may be preferred to avoid possible GA complications. Various RA techniques, such as thoracic epidural anesthesia, paravertebral, intercostal blocs, intrapleural blocks, or newly described PECS (pectoral nerve block type) 1 and 2, SAP (serratus anterior plane) block, and ESP (Erector spinae plane) blocks have been applied for breast surgery in high-risk patients [3]. Thoracic paravertebral block (TPVB) has been used recently, and ultrasound (US) imaging has become more widespread. Its safety and technical convenience have increased [4]. The technique is based on injecting the local anesthetic solution into the triangular-shaped paravertebral space limited by the pleura, costotransverse ligament, and transverse process. Depending on the indication, the procedure can be performed in single or multiple intervals [3, 4].
We aimed to present anesthesia management with unilateral MRM with a TPVBunder remifentanil sedation in a PVpatient with multiple comorbidities.
Case description
An 81-year-old female had a history of PV, coronary artery disease (1 stent), hypertension, chronic pulmonary thromboembolism, pulmonary hypertension (systolic pulmonary arterial pressure (PAP) was 45-50 mmHg classification II), left ventricular concentric hypertrophy, and left ventricular diastolic dysfunction, dyslipidemia, depression, and type 2 diabetes mellitus. The patient uses warfarin 5 mg, rosuvastatin 40 mg, metoprolol 25 mg, metformin 1000 mg, irbesartan 300 mg, sertraline 25 mg, and methylprednisolone 16 mg once a day for treatment purposes. The patient was advised to continue using all her medications in the preoperative period and to discontinue warfarin five days before.
She had dyspnea, and her exercise capacity was approximately 3 METs. On physical examination, there were hyperemic ulcerated lesions on the soft palate, and mouth opening was sufficient (Figure 1). Stridor was present during labored inhalation and exhalation. Chest auscultation revealed a systolic murmur in the tricuspid region, clicks in the prosthetic valve, and slightly prolonged expiration. Also, an ulcerated lesion covering the soft palate and right palatoglossal arch and two eroded skin sites on the left scapula were noted.
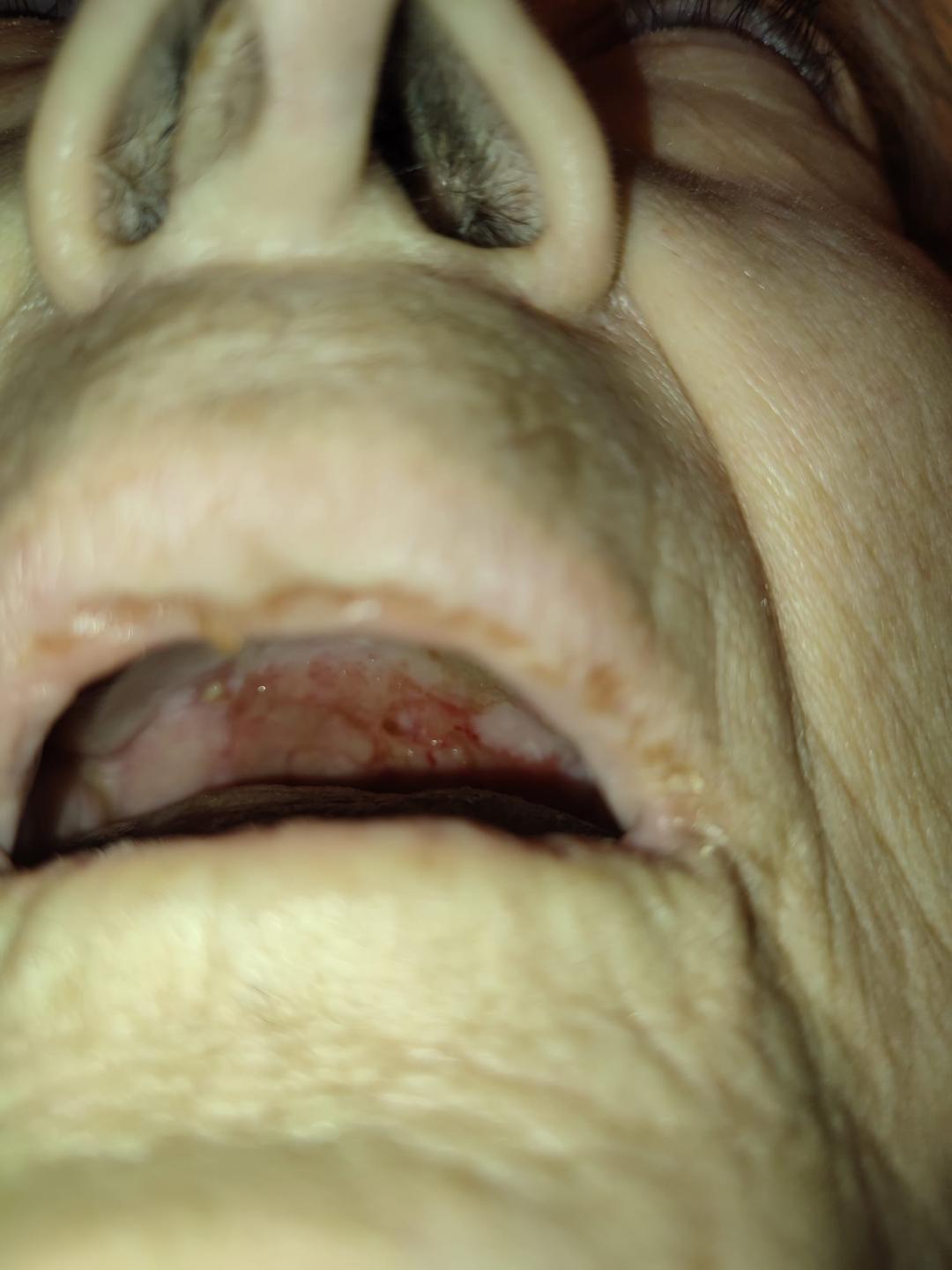
Figure 1
The patient's blood urine nitrogen was 35 mg/dL, creatinine was 1.22 mg/dL, platelet 161x103/mL, and international normalized ratio (INR) was 1.3. Other values, including plasma albumin levels, were within the normal ranges. The electrocardiogram (ECG) showed sinus bradycardia (54/min.) with a right bundle branch block (RBBB). In the transthoracic echocardiography (TTE), ejection fraction (EF) was 59%, left ventricular diastolic dysfunction, tricuspid annular plane systolic excursion (TAPSE) was 18, and systolic PAP was 45-50 mmHg was detected. In addition, the patients had 3/4 tricuspid failure, 1/4 pulmonary failure, and 2/4 mitral regurgitations.The patient's effort capacity was evaluated as class II. The cardiologist evaluated the operation as high risk and intermediate risk by the pulmonologist. The patient's American Society of Anesthesiologists (ASA) physical classification class III and Mallampati score II. Fiberoptic laryngoscopy performed by the ENT (Ear Nose Throat) team revealed supraglottic stenosis and hyperemic ulcerated lesions with mucoid discharge. No significant worsening in the stenosis was observed compared to the examination a year prior. This report, images, and verbal and written informed consent were published with consent from our patient.
All risks and the planned anesthesia method for the patient were detailed to them. Due to shortness of breath on exertion, we did not apply premedication to our patients. After a short identity check and confirmation of the operation room, special monitoring was applied to the patient with PV. The 3-lead electrocardiogramelectrode was cleaned of adhesive coating and fixed to the wrists and left ankle with non-elastic bandages. The 20 G intravenous (IV) line was also fixed with bandages.The arm was padded with cotton dressing before applying a noninvasive blood pressure (NIBP) cuff (Figure 2). A nonadhesive pulse oximeter probe was also used. After standard monitorization, heart rate was 52/min, blood pressure was 160/85 mmHg,and peripheral oxygen saturation (SpO2) was 90%. Nasal cannula tubes were wrapped with cotton in areas directly touching the skin (Figure 3). At this stage, IV administered a prophylactic dose of cefazolin (2000 mg) and a 'stress dose' of dexamethasone (8 mg).

Figure 2

Figure 3
The TPVB was chosen as the primary anesthesia method for the surgery to avoid any instrumentation of the upper airways. The block site was cleaned with an antiseptic solution, and a lubricant gel was applied generously to prevent the skin from being rubbed off by the US transducer. In a sitting position, a visualization of distal tips of transverse processes was achieved via a 6-12 MHz linear US transducer. The transducer was placed parasagittally, and the needle pointed in the caudad direction. Using the in-plane technique, an echogenic 22-gauge Touhy needle (StimuplexA) 80 mm short bevel needle was inserted at the steep 80-degree angle to the paravertebral space. The injection site was 5 cm to the lesion onthe left scapula, and 5 ml of 0.5% bupivacaine was injected in each paravertebral space from T2 to T6 (Figure 4).
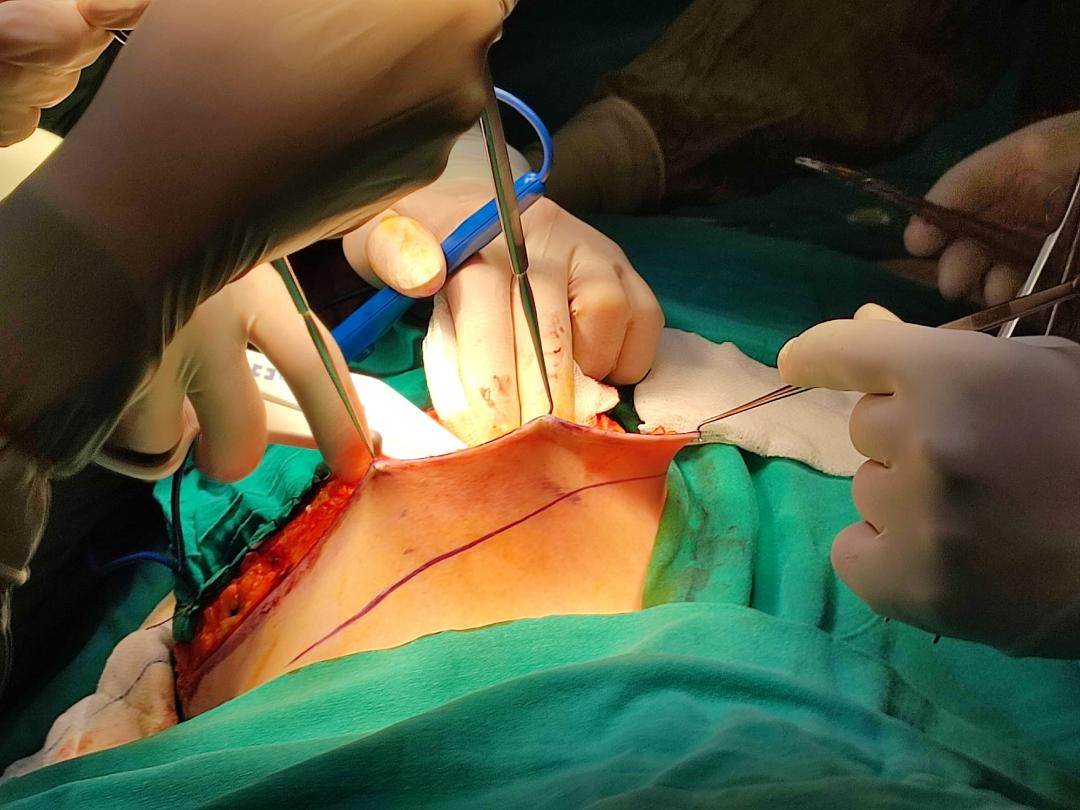
Figure 4
The surgery was started 20 minutes after the paravertebral dose was given in the patient whose sensory block level height of T2 to T6 was achieved unilaterally, evaluated by pinprick test, and Bromage score was 0. The patient, who was observed to tolerate the incision well, was administered nasal 2 L/min oxygen and remifentanil via IV infusion for sedation throughout the surgery, and the dose range was titrated according to hemodynamic changes and the Ramsey sedation scale. Throughout the surgery, the patient's Ramsay sedation scale was evaluated as 3, and the patient was hemodynamically stable and quite comfortable. The duration of the operation was around 155 minutes. All breast tissue and the armpit contents on the same side (fat tissue and sentinel lymph nodes) were removed (Figure 5). During the monitoring period, the patient did not mark any side effects, breakthrough pain, nausea, or vomiting. At the 4th hour after the surgery, the patient reported that she did not feel any pain, and after the 12th hour, when the visual analog scale was 6, paracetamol 1000 mg and 50 mg meperidine wasadministered in an IV. In the following days, no rescue analgesic or antiemetic medication was required. Oral feeding was started on the patient eight hours after surgery. The patient was discharged on the fourth day without any complications.

Figure 5
Discussion
The primary purpose of the anesthesia management of our case was to avoid airway instrumentation as much as possible due to the expected difficult intubation due to upper airway stenosis and the possibility of worsening of the lesions and, in the worst case, even the need for tracheostomy [1, 2].We have shown that TPVB is a logical, effective, and safe alternative to GA for MRM. In essence, we preferred the TPVB over GA as they included increased surgical stress response, opioid requirement, postoperative cardiopulmonary complications, and avoidance of airway challenges. The advantages of the TPVB include hemodynamic stability, lower postoperative pulmonary complications, effective postoperative analgesia, lower analgesic consumption, lower frequency of postoperative nausea and vomiting, early nutrition and mobilization, and shorter hospital stays [4- 6].
Comprehensive preoperative evaluation, identification of risks, and optimization are highly critical for correct anesthesia management in elderly patients with PV and multiple comorbidities who will undergo surgery. Due to the increased risk of mortality and morbidity in the perioperative period in these patients, preoperative evaluation should primarily focus on the extent and effects of the disorder caused by airway lesions due to PV [2].
Preoperative precautions to be taken in patients with PV can prevent morbidity and mortality. The points we pay special attention to in our patient are as follows:
• In these patients, applying pressure to the skin causes blisters or erosion, and placement of monitoring devices, IV lines, and blood pressure cuffs during airway interventions requiressignificant care [1,2]. We avoided the use of alcohol swabs before the insertion of the IV cannula. Perioral scar lesions may restrict mouth opening.
• Intraoral lesions are present in 75% of cases. Endotracheal intubation is dangerous in these patients due to existing ulcerations, blistering, and edema formation [1, 2], and we preferred TPVB in our patient to prevent these possible complications.
• Extensive aspiration should be avoided to prevent mucosal trauma. In case of possible intubation, lubrication of the laryngoscope and tracheal tube, gentle laryngoscopy, and use of a small tracheal tube should be preferred [1].
• Pharmacological management of patients with PV is also essential. The primary treatment of PV consists of local or systemic corticosteroid therapy [1,2]. We continued dexamethasonetreatment during and after surgery to reduce the risk of possible aggravation and Adisonian crisis.
• Malnutrition may occur due to lesions in the mouth, and fluid and electrolyte imbalances may occur due to skin lesions. It is vital to ensure perioperative hydration in these patients [2]. We gave our patient IV fluids according to her hourly urine output, consideringher existing cardiac comorbidities.
• Based on this information, choosing sedoanalgesia and/or RA may be more appropriate [2,4,6].
Since our patient was high-risk, ASA III, and had an elderly patient with PV and multiple comorbidities, we mainly applied TPVB to provide anesthesia and analgesia in the intraoperative and postoperative periods to avoid possible complications of GA. The nerves going to the breast must be understood in detail to ensure successful RA in the breast. The breast skin, mammary gland, and nipple are supplied by the T2-T6 intercostal nerves, which the TPVB sufficiently blocks [3- 6]. We preferred to support it with TPVB to provide a more comfortable analgesia for the patient. TPVB has a high success rate and minimal complication incidence when carried out by an anaesthesiologist knowledgeable and experienced in peripheral nerve blocks under US guidance. Our decision to stay with TPVB only was based on our desire to avoid GA whenever possible. Therefore, we used an appropriate dose of local anesthetic and did not observe any complications related to local anesthetic.
We could not find many cases in the literature where the combination of TPVB and sedation was applied. We chose TPVB as the primary anesthesia technique for our patient, as it allows intensive blocking of the most significant area with a high-concentration local anesthetic solution, compared to the PECS, SAP, and ESP used [3- 5]. Pawa and colleagues reported that they performed a prospective observational case series consisting of 16 breast cancer surgeries conducted under TPVB plus pectoral nerve block; 15 of the 16 cases were completed under sedation and RA, and one was converted to GA. In these patients, surgeons reported being 'extremely satisfied' or 'satisfied' with the technique after each procedure and that combining TPVB plus pectoral nerve block with intraoperative sedation was an appropriate technique in breast surgery [7]. Simpson and colleagues reported that in a case series of 28 elderly patients with multiple comorbidities in whom TPVB and sedation were used in breast surgery, they performed single or multi-level injections and used propofol or remifentanil for sedation, and prilocaine supplementation was applied by the surgical team when necessary. At the end of this study, they stated that TPVB with sedation and US guidance is an effective and reliable form of anesthesia in breast surgery [8].
Contrary to these two studies, we performed TPVB with injection only between T2-T6 in our patient before surgery, and we completed the surgery by applying remifentanil infusion for sedation during the surgery, without PECS block and any routine surgical local anesthetic supplementation. One of the main advantages of our technique is that it is safe and facilitates ambulatory surgery in patients with significant multiple comorbidities, especially in patients with significant air lesions such as PV. Moreover, when performed in conjunction with TPVB and sedation, it was highly acceptable to the patient and was met with high satisfaction by the surgical team. We observed that TPVB provided excellent analgesia in the first 4 hours of the postoperative period in our patient, even though mastectomy and axillary node cleaning were performed at the same time.We think that TPVB alone, combined with intraoperative sedation, may be an appropriate technique for patients with multiple comorbidities and PV undergoing breast surgery.
The TPVB technique has some limitations in patients undergoing breast surgery. First, the perioperative period is short, and the patient's acceptance of this technique may change as the surgery time increases. Secondly, the surgery lasted 155 minutes in our patient, and although she did not routinely need local anesthetic supplementation, it may not be possible for this to happen in other patients. Although no complications were detected, proving the technique is safe for a single patient is insufficient.In light of the literature, we suggested the TPVB for oncologic breast surgeries in high-risk patients and PV. However, the TPVB technique's effectiveness, reliability, practicality prospective, and large and randomized control trials are needed. Despite these potential limitations, this technique may provide an exciting avenue of discovery in patients with multiple comorbidities and specific diseases such as PV, and we think it will contribute significantly to the greater adoption of this technique by anesthesiologists.
Conclusion
In summary, considering the advantages and disadvantages of GA, particularly in patients with high-risk having multiple comorbidities and PV, we suggest that TPVB can be used combined with sedation as an effective, feasible, and safe method for hemodynamic stability in intraoperative and postoperative pain control in patients undergoing oncologic breast surgeries and in reducing the need for postoperative analgesic use and postoperative complications. For patients with PV and multiple comorbidities, comprehensive preoperative preparation of the patient with a multidisciplinary approach, adequateprotective measures, optimization, correct cooperation with the surgical team, and close postoperative follow-up are essential in preventing complications.
Author Contributions
Nursultan Akmatov: Conceptualization; Investigation; Writing-original draft; Writing–review& editing.
İrem Yıldız: Conceptualization; Investigation; Corresponding Author
Nedim Çekmen: Conceptualization; Supervision; Writing-review&editing.
Sedat Yıldırım: Conceptualization; Supervision; Writing-review&editing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
None
Conflicts of interest
There are no conflicts of interest
References
- Porro AM, Seque CA, Ferreira MCC, Enokihara MMSES (2019) Pemphigus vulgaris. Anais Brasileiros de Dermatologia 94: 264-278.
- Roberta L Hines, Stephanie B Jones (2021) Stoelting's Anesthesia and Co-Existing Disease. (8th Edn) Elsevier 498-500.
- Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB (2017) Perioperative breast analgesia: A qualitative review of anatomy and regional techniques. Reg Anesth Pain Med 42: 609-631.
- FitzGerald S, Odor PM, Barron A, Pawa A (2019) Breast surgery and regional anaesthesia. Best Pract Res Clin Anaesthesiol 33: 95-110.
- Batra RK, Krishnan K, Agarwal A (2011) Paravertebral block. J Anaesthesiol Clin Pharmacol 27: 5-11.
- Pei L, Zhou Y, Tan G, Mao F, Yang D, Guan J, et al. (2015) Ultrasound-assisted thoracic paravertebral block reduces intraoperative opioid requirement and improves analgesia after breast cancer surgery: a randomized, controlled, single-center trial. PLoS ONE 10: 1-15.
- Pawa A, Wight J, Onwochei DN, Vargulescu R, Reed I, et al. (2018) Combined thoracic paravertebral and pectoral nerve blocks for breast surgery under sedation: a prospective observational case series. Anaesthesia 73: 438-443.
- Simpson J, Ariyarathenam A, Dunn J, Ford P (2014) Breast surgery using thoracic paravertebral blockade and sedation alone. Anesthesiology Research and Practice 2014: 127467.