Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/128
Research Letter OPEN ACCESS
Efficacy of Dexmedetomidine Infusion to Attenuate Hemodynamic Response and Opioid Sparing Properties During Wide Excision of Carcinoma Tongue
Abhijit Nair1*, MD, Hemanth Kumar Nemade2, MS, Jonathan Gondi2, MDS, Basanth Kumar Rayani1, DA, DNB
1Department of Anaesthesiology, Basavatarakam Indo-American Cancer Hospital and Research Institute, Road No. 10, Hyderabad-500034, Telangana State, India
2Department of Head and Neck Surgical Oncology, Basavatarakam Indo-American Cancer Hospital and Research Institute, Road No. 10, Hyderabad-500034, Telangana State, India
Abhijit Nair, Department of Anaesthesiology, Basavatarakam Indo-American Cancer Hospital and Research Institute, Road No. 10, Hyderabad-500034, Telangana State, India, Tel: 91-040-23351245; Fax: 91-040-2354 2120; E-mail: abhijitnair95@outlook.com
Editor: Renyu Liu, MD, PhD, Professor, Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, Center of Penn Global Health Scholar, Director of Stroke 120 Special Task Force, Chinese Stroke Association, 336 John Morgan Building, 3620 Hamilton Walk, Philadelphia, PA 19104, USA, Phone: 2157461485, Fax: 2153495078, E-mail: RenYu.Liu@pennmedicine.upenn.edu
Received: June 22, 2020 | Accepted: August 01, 2020 | Published: August 05, 2020
Citation: Nair A, Nemade HK, Gondi J, Rayani BK. Efficacy of Dexmedetomidine Infusion to Attenuate Hemodynamic Response and Opioid Sparing Properties During Wide Excision of Carcinoma Tongue. Transl Perioper & Pain Med 2020; 7(4):288-290
Head and neck surgical resections involve accelerated hypertensive surges especially during resection of tumor [1]. When wide local excision (WLE) of tongue lesion is performed for carcinoma tongue, it is associated with significant hemodynamic response. During the incision there is accelerated hypertension, tachycardia and surgical bleeding. This unwanted hemodynamic response in not desirable in hypertensive patients, patients with coronary and cerebrovascular disease. This is addressed using incremental doses of opioids, increasing depth of anesthesia, IV (intravenous) beta blockers, propofol boluses or nitroglycerine infusion [2]. This addresses the hemodynamic issues but is associated with hypotension once the glossectomy is done. This requires use of vasopressors and unnecessary stay in a dependency unit for stabilizing hemodynamics.
Dexmedetomidine is a centrally acting α2 agonist which causes sympatholysis and thereby attenuates hemodynamic response to intubation, surgical incision [3]. We hypothesized that by using dexmedetomidine infusion in recommended doses during WLE of tongue lesions there could be attenuation of hemodynamic response during surgical incision and also would reduce intraoperative opioid consumption.
After Institutional Ethics Committee approval, 20 American Society of Anesthesiologists'-physical status (ASA-PS) I-II patients with carcinoma tongue scheduled for WLE of tongue lesion were enrolled randomly for this study. One group was offered standard intraoperative management (control group) while other (Test group) Dexmedetomidine infusion was used. Demography details (age, gender, weight, ASA-PS) is shown in table 1. An informed consent was obtained from all patients. All patients underwent as thorough pre-anesthesia checkup and were posted for proposed surgery once certified fit by the Anesthesiologist. After confirming nothing by mouth status for 6 hrs, patients were shifted to operating room. An appropriately sized IV cannula was secured and essential monitoring was established (pulse oximeter probe for oxygen saturation, noninvasive blood pressure cuff and electrocardiography using lead II, V5). Standard general anesthesia technique used was 0.03 mg/kg midazolam, 1.5 μg/kg fentanyl and 2-2.5 mg/kg of propofol, all IV. In both arms of study, neuromuscular blockage was achieved using 0.1 mg of IV vecuronium and airway was secured with appropriately sized flexometallic endotracheal tube placed nasally which was confirmed using end-tidal carbon dioxide trace. Anesthesia was maintained with oxygen/medical air (fresh gas flow of 1 L) and isoflurane titrated to a MAC of 1. All patients received 0.1 mg dexamethasone after induction and 1 gm paracetamol IV during surgical closure. 10 patients received standard general anaesthetic as described below. 10 patients in test group received 1 μg/kg dexmedetomidine over 15 minutes (loading) followed by 0.5 μg/kg/hr till glossectomy was performed. In both groups, patients received another 50 μg boluses of fentanyl if hemodynamics (heart rate, systolic and mean blood pressure) increased from 20% of baseline intraoperatively.
Table 1: Demography details, and comparison of intraoperative fentanyl consumption.
| Variables | Control group | Test group | P value |
| Age (years) | 51 ± 11.17 | 50.3 ± 13.16 | 0.449 |
| Weight (kg) | 63.6 ± 10.65 | 66.4 ± 14.40 | 0.307 |
| Gender (M/F) | 9/1 | 6/4 | 0.121 |
| ASA- PS (I/II) | 4/6 | 2/8 | 0.329 |
| Intraoperative fentanyl (μg) | 200 ± 20.41 | 129.5 ± 23.14 | < 0.00001* |
ASA-PS: American society of Anesthesiologists’-physical status
*- P-value less than 0.05 was considered statistically significant.
Appropriate statistical tests were employed for analysis of data from both groups. Continuous data was expressed as mean ±standard deviation or median and interquartile range whichever was applicable and analyzed using unpaired t-test. Categorical data was expressed as absolute numbers and analyzed using Chi-Square test. p-value of less than 0.05 was considered statistically significant. Statistical analyses were executed by GraphPad Prism 5 for Windows (GraphPad Software, La Jolla, CA, USA).
Intraoperative hemodynamics and total fentanyl consumption were noted and compared in both groups. The demographic data were comparable in both groups. Hemodynamics were stable in dexmedetomidine group compared to standard group (Figure 1). There was a significantly lesser use of intraoperative fentanyl in patients who received dexmedetomidine (129.5 ± 23.2 μg) than in control group (200.0 ± 20.4 μg, P < 0.0001).
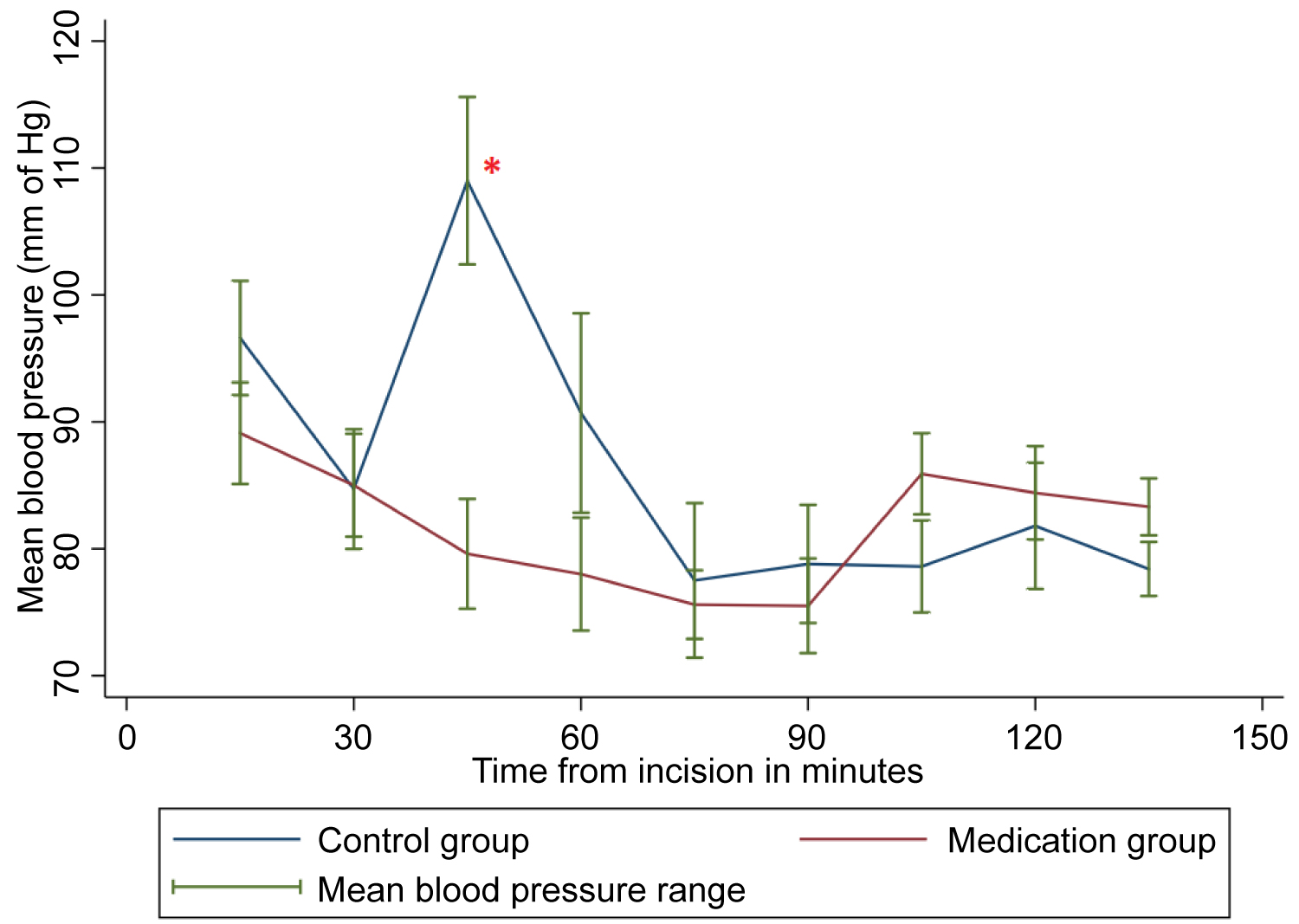
Figure 1: Comparison of the correlated mean blood pressure in the patients undergoing wide local excision of the tongue.
*- denotes statistical significance
Intraoperative hypertensive crisis is undesirable [4]. The causes are many like inadequate analgesia, inadequate depth of anesthesia, instrumentation or handling painful structures. This crisis can have adverse perioperative outcomes leading to adverse cardiovascular and cerebrovascular events, bleeding, and increased mortality in high risk surgeries. Continuing scheduled dose of anti-hypertensives on the day of surgery is important and should be clearly mentioned in preoperative instructions [5]. Medications like diuretics, angiotensin receptor blockers and ACE-inhibitors needs to be omitted on the day of surgery but can be replaced with any calcium channel blocker. Dexmedetomidine is an alpha 2 adrenergic receptor agonist which is ten times more selective for alpha 2 receptor than clonidine [6]. Preoperative loading dose of dexmedetomidine has shown to effectively obtund intubation response and also confers intraoperative hemodynamic stability [7]. Several studies have attested the efficacy of dexmedetomidine in providing stable intraoperative hemodynamics, reduced perioperative and volatile anesthetic/opioid use and as an adjunct to neuraxial and peripheral nerve block [8-11]. Hypotension and bradycardia after the loading dose of dexmedetomidine can be easily treated managed with co-loading of crystalloids, anticholinergics like glycopyrrolate or drugs like ephedrine or mephentermine in small aliquots.
The findings of the present study are limited by small sample size which limits a detailed statistical analysis of the available data. Still with this limited data, we could demonstrate that intraoperative hemodynamics were well maintained with lesser intraoperative fentanyl consumption in dexmedetomidine group compared to control group. Well-designed, adequately powered randomized study needs to be done to establish the role of dexmedetomidine in attenuating hemodynamic response to glossectomy and to reduce perioperative opioid consumption.
Conflicts of Interest
None
Acknowledgements
None
References
- Anjum Ahmed-Nusrath, Anaesthesia for head and neck cancer surgery, BJA Education, Volume 17, Issue 12, December 2017, Pages 383–389, https://doi.org/10.1093/bjaed/mkx028.
- Aronow WS. Management of hypertension in patients undergoing surgery. Ann Transl Med. 2017; 5:227.
- Kim JK. An introduction to the various role of dexmedetomidine. Korean J Anesthesiol. 2016; 69:543-44.
- Lonjaret L, Lairez O, Minville V, Geeraerts T. Optimal perioperative management of arterial blood pressure. Integr Blood Press Control. 2014; 7:49-59.
- Pai SL, Chadha RM, Irizarry-Alvarado JM, Renew JR, Aniskevich S.Pharmacologic and Perioperative Considerations for Antihypertensive Medications.Curr Clin Pharmacol. 2017; 12:135-140.
- Naaz S, Ozair E. Dexmedetomidine in current anaesthesia practice- a review. J Clin Diagn Res. 2014;8:GE01-GE4.
- Lee CW, Kim M. Effects of preanesthetic dexmedetomidine on hemodynamic responses to endotracheal intubation in elderly patients undergoing treatment for hypertension: a randomized, double-blinded trial. Korean J Anesthesiol. 2017; 70:39-45.
- Obara S. Dexmedetomidine as an adjuvant during general anesthesia.J Anesth. 2018; 32:313-15.
- Nair A. Less explored off-label indications of dexmedetomidine. Korean J Anesthesiol. 2017; 70:361-2.
- Tang C, Xia Z. Dexmedetomidine in perioperative acute pain management: a non-opioid adjuvant analgesic. J Pain Res. 2017; 10:1899-1904.
- Bohringer C, Liu H. Is It Time for an Expanded Role of Dexmedetomidine in Contemporary Anesthesia Practice? - A Clinician's Perspective. Transl Perioper Pain Med. 2018;5:55-62.